20 Little-Known Steps to Outsmart Chronic Inflammatory Demyelinating Polyneuropathy
Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) may not be a household name, but for those living with it, the effects are unmistakable—tingling, weakness, numbness, and the steady erosion of mobility. This rare autoimmune disorder causes the body’s immune system to mistakenly attack the myelin sheath, the protective coating around nerve fibers. As that insulation breaks down, communication between nerves and muscles falters, leading to progressive, often frustrating symptoms. While treatment often involves immunotherapy or steroids, navigating CIDP successfully means going beyond the basics. Lifestyle choices, dietary tweaks, recovery techniques, and strategic habits can all make a measurable difference. That’s why we’ve expanded our guide to include 20 Little-Known Steps to Outsmart Chronic Inflammatory Demyelinating Polyneuropathy—insightful, practical strategies designed to help you take back control. Whether you’ve just been diagnosed or are deep into your CIDP journey, these overlooked steps could be the key to managing symptoms more effectively and living with greater strength and stability.
1. Diagnostic Tests

It can be difficult for a physician to narrow down a diagnosis of chronic inflammatory demyelinating polyneuropathy in an individual who presents with symptoms characteristic of this rare neurological disorder. An individual who has symptoms of chronic inflammatory demyelinating polyneuropathy may be brushed off until their symptoms become so pronounced that they interfere with everyday activities and responsibilities. The only diagnostic tests used specifically to make a chronic inflammatory demyelinating polyneuropathy diagnosis are a spinal tap, nerve biopsy, and electromyography. A chronic inflammatory demyelinating polyneuropathy patient may exhibit abnormally high levels of certain proteins in their cerebrospinal fluid that can be detected with the use of a spinal tap procedure. Patients will also present with a pattern of multifocal demyelination when they undergo a nerve conduction study or electromyography.
2. Plasmapheresis

Plasmapheresis is a treatment method where the patient's blood is removed from the body and plasma is separated from the rest of the blood inside of a specialized machine. The plasma portion of the blood is replaced with a mixture of saline and albumin before it is mixed with the rest of the blood and sent back into the patient's body. The mechanism of this type of blood filtering is similar to what occurs with dialysis. The objective of this treatment is to remove the components of the blood responsible for eliciting the inappropriate attack on the healthy myelin sheathing. Numerous different types of autoantibodies are implicated in chronic inflammatory demyelinating polyneuropathy. The most common autoantibodies identified in affected individuals include antibodies against peripheral myelin protein two or PMP2, peripheral myelin protein 22 or PMP22, and myelin protein zero or MPZ. The regular removal of these antibodies from an affected individual's blood via plasmapheresis can help alleviate symptoms of CIDP.
3. Corticosteroids

Symptoms of chronic inflammatory demyelinating polyneuropathy are caused by an abnormal reaction of the patient's immune system where it attacks and destroys the cells that make up the myelin sheath around the nerves. Corticosteroids are a type of medication that changes mediator functions in the part of the body where the immune system is attacking its own tissues and alters the synthesis of proteins in the cells to suppress the immune responses and inflammation. In the cases of many individuals with autoimmune conditions, corticosteroids are used as the first-line treatment to help the patient's symptoms go into remission. Corticosteroids are known to be effective for the treatment of chronic inflammatory demyelinating polyneuropathy in most individuals, but may not work for everyone. Other treatment methods are often used alongside corticosteroids in patients with severe CIDP. Some of the most common corticosteroids used in individuals with CIDP include intravenous methylprednisolone, oral daily prednisone, and pulsed dexamethasone.
4. Intravenous Immunoglobulin
Intravenous immunoglobulin is an infusion composed of small portions of IgM and IgA and a more significant portion of heterogeneous human IgG. In each batch of intravenous immunoglobulin, there are blood components that have been prepared from the serum of between one and fifteen thousand human donors. This type of solution can provide a wide array of antibodies with the capacity to neutralize the components of the immune system causing damage to the affected individual's myelin sheathing. The exact mechanism of action that has proven to show improvements in the symptoms of CIDP is not clear, but it is thought to involve the inhibition of the autoantibody action on the healthy tissues. Intravenous immunoglobulin has been able to promote the remyelination of lacking nerves, which may reverse some of the damage done by the affected individual's rogue immune system.
5. Physiotherapy

As we know, chronic inflammatory demyelinating polyneuropathy is an illness known to cause progressive muscle weakness. This malfunction can make it difficult for a patient to perform everyday tasks like walking. Once the illness is under control, the atrophy or muscle wasting that occurs in the individual can be reversed as long as there is no permanent damage to the nerves. Even individuals who do have permanent nerve damage due to CIDP may choose to undergo physiotherapy to help maximize their movement potential and improve their quality of life. Physiotherapy is the utilization of movement and exercises to help re-strengthen muscles, improve mobility, increase range of motion, and rehabilitate impaired muscles. Physiotherapy is merely a part of a patient's treatment regimen, as it does not provide any curative qualities to the autoimmune disorder itself. Physiotherapy can help alleviate symptoms and prevent some complications of CIDP, but it does not stop the patient's immune system from attacking the protective myelin around the nerves.
6. Immunotherapy

If corticosteroids are not an option for a chronic inflammatory demyelinating polyneuropathy patient, immunotherapy may be added to help mediate their symptoms. Immunotherapy is a treatment typically used to slow down the actions of an individual's immune system. This mechanism is difficult to achieve because it involves leaving some parts of the patient's immune system active and functioning, while selectively deactivating the parts of the immune system causing the CIDP symptoms. Other methods in immunotherapy used to treat autoimmune disorders like CIDP are not specific to the particular parts of the immune system that cause the specific disorder. This non-specificity results in adverse side effects some patients may not be able to handle. Immunotherapy is the manipulation of the individual's immune system responses to treat the imbalance without causing significant adverse side effects.
7. Stem Cell Transplant
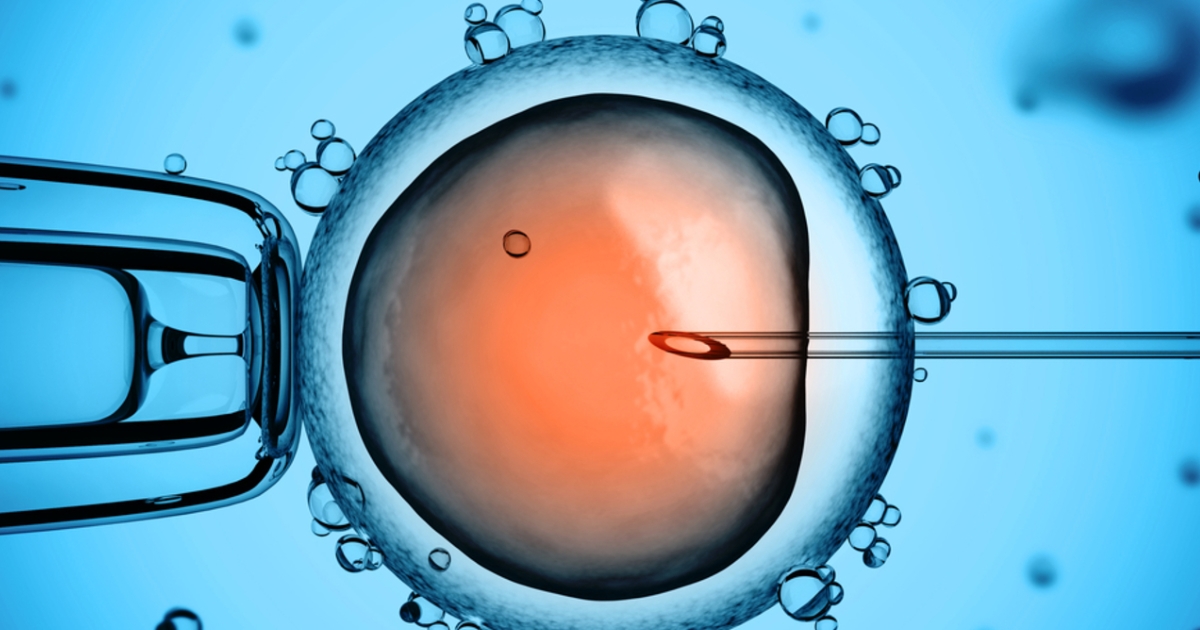
Some individuals affected by chronic inflammatory demyelinating polyneuropathy may benefit from the use of a hematopoietic stem cell transplant. A hematopoietic stem cell transplant is a procedure where stem cells are used to rebuild a patient's immune system. First, high doses of ATG and cyclophosphamide are used to eradicate all of the existing cells in the immune system of a chronic inflammatory demyelinating polyneuropathy patient. Next, stem cells are introduced to the affected individual's body. These stem cells essentially repopulate and rebuild the patient's immune system with the hope it will no longer attack healthy tissues in the body. A new and healthy immune system that results from a stem cell transplant has proven to cure chronic inflammatory demyelinating polyneuropathy in some patients who had no success with other methods of treatment.
8. Immunosuppressants

A chronic inflammatory demyelinating polyneuropathy patient may need to take immunosuppressants as part of their treatment regimen to relieve symptoms. An immunosuppressant is a type of medication used to lower or decrease the activity of an affected individual's immune system. Disorders caused by the inappropriate and abnormal attack of the immune system on the healthy tissues of an individual's body can sometimes be mediated when the immune system is downregulated in its activities. Immunosuppressants work by reducing the overall activity of the patient's immune system. It is important to consider an individual becomes more vulnerable to infections and abnormal cell growth in their body when they take immunosuppressants. In some cases, a patient may be treated with an immunosuppressant in conjunction with other medications, like corticosteroids. Azathioprine, methotrexate, cyclophosphamide, mycophenolate, and cyclosporine are the most common immunosuppressants utilized in the treatment of chronic inflammatory demyelinating polyneuropathy.
9. Patient Prognosis

The prognosis of a chronic inflammatory demyelinating polyneuropathy patient is difficult to determine because it presents with a variety of different clinical evolutions and patterns. A young patient who has less pain at the onset of their chronic inflammatory demyelinating polyneuropathy will have a better long term outcome than an older patient who experiences more pain. Poor functional outcome in an individual affected by chronic inflammatory demyelinating polyneuropathy is associated with the finding of axonal loss on a nerve biopsy. Individuals affected by the chronic progressive course of chronic inflammatory demyelinating polyneuropathy are known to have a worse prognosis than patients affected by the relapsing course of chronic inflammatory demyelinating polyneuropathy. Chronic inflammatory demyelinating polyneuropathy patients respond in various ways to different treatment methods. The efficacy of treatment is highly dependent upon how progressive the disorder is at the time of diagnosis.
10. Connection To Guillain-Barre Syndrome

Guillain-Barre syndrome is a condition where an individual's peripheral nerves develop an acute inflammatory disease characterized by symptoms that develop suddenly and progress rapidly. This syndrome is caused by an inappropriate and abnormal reaction by an individual's immune system, where it attacks the protective myelin sheathing around the nerves. Most individuals affected by Guillain-Barre syndrome recover without a problem and do not experience long-term or persistent symptoms. However, some Guillain-Barre syndrome patients may experience a permanent alteration of their immune system, where it continues to destroy myelin sheaths slowly and progressively. This alteration that occurs in an affected individual's immune system causes long-term symptoms that can be characterized as chronic inflammatory demyelinating polyneuropathy.
11. Vitamin B12 Optimization

Vitamin B12 plays a critical role in nerve health and myelin production, making it essential for anyone with CIDP. A deficiency in B12 can worsen symptoms like numbness, weakness, and poor coordination. Even borderline levels may aggravate nerve dysfunction in patients already battling demyelination. Regular blood tests can identify deficiencies early. Supplementation—either oral or injectable—can restore optimal levels and support nerve repair. Choose methylcobalamin over cyanocobalamin for better absorption and neurological benefit. Discuss dosing with your neurologist, especially if you're also taking immunosuppressants, which can impair absorption. B12 isn’t a cure, but it's a valuable neuro-supportive tool.
12. Anti-Inflammatory Diet Focus

While no diet can reverse CIDP, certain eating patterns can help reduce systemic inflammation that may worsen symptoms. An anti-inflammatory diet—rich in leafy greens, berries, fatty fish, turmeric, and olive oil—can support immune balance and protect nerves. Reducing sugar, processed foods, and trans fats may also ease fatigue and flare severity. Omega-3s from salmon, flaxseed, and walnuts have specific neurological benefits. Gluten and dairy may be inflammatory for some, so elimination trials with a dietitian’s guidance can help. Think of your plate as a daily decision toward healing: small shifts in food can lead to measurable changes in function.
13. Compression Garments for Stability

CIDP patients often experience weakness, especially in the lower limbs, which can lead to instability and balance issues. Compression socks or sleeves can improve proprioception—your body’s sense of position—and support blood flow to fatigued limbs. While they won't correct nerve damage, these garments can reduce swelling, delay muscle fatigue, and add a sense of control over unsteady legs or arms. Athletes use them for similar reasons: stability and endurance. For CIDP patients, it's about maintaining mobility safely and confidently. Choose moderate compression and consult a physical therapist to find the best fit and function.
14. Adaptive Exercise (Not Just Physical Therapy)

Exercise isn't one-size-fits-all with CIDP—but it's essential. Beyond formal physical therapy, adaptive exercises like water aerobics, resistance band routines, and chair yoga can maintain muscle tone and prevent contractures. These low-impact options reduce joint stress and allow for customization based on energy levels. Even small daily movements can improve blood flow to nerves and reduce deconditioning. Avoid overexertion, and listen to your body—pushing through fatigue may worsen symptoms. Track your energy and symptom patterns to time your movement wisely. Movement is medicine—but only when matched to your current capacity.
15. Sleep Hygiene as a Recovery Tool

Poor sleep can intensify nerve pain, impair immune regulation, and reduce your capacity to heal. Unfortunately, CIDP symptoms—like tingling or muscle cramps—can also disrupt sleep. That’s why prioritizing sleep hygiene is key. Stick to a regular bedtime, reduce blue light exposure in the evenings, and avoid stimulants late in the day. Create a wind-down ritual that includes stretching or a warm bath to relax overactive nerves. Discuss sleep disorders with your doctor—sleep apnea is more common in autoimmune conditions. Restorative sleep helps regulate inflammation, stabilize mood, and optimize nerve repair. It's more powerful than it sounds.
16. Psychological Support and Pain Coping Tools

Living with a chronic condition like CIDP can take a serious toll on mental health. Anxiety, depression, and frustration are common—but rarely addressed. Therapy (especially CBT) can help reframe pain, manage fatigue-related guilt, and develop tools for emotional regulation. Mindfulness-based stress reduction has been shown to reduce chronic pain perception and support nervous system regulation. Support groups, whether online or in person, offer community validation and shared insight. Mental health is physical health when it comes to chronic neurological illness—your nervous system functions best when stress is under control. Make space for your emotional well-being.
17. Functional Neurological Rehab

Beyond traditional physiotherapy, functional neurological rehab (FNR) focuses on restoring lost function through targeted neural retraining. It uses sensory re-integration, balance work, and specific movement patterns to stimulate dormant pathways. For CIDP patients with lingering deficits, FNR may offer improvement even when standard therapy has plateaued. Some clinics integrate neurofeedback, mirror therapy, or cranial nerve stimulation. These techniques aim to rebuild the brain-body connection, compensating for impaired peripheral signaling. It’s especially helpful for those with partial remyelination or incomplete recovery. While still emerging, FNR offers hope for regaining independence through rewiring—not just strengthening—your nervous system.
18. Regular Neuropathy Screenings

CIDP is a progressive condition, and monitoring is critical. Beyond symptom tracking, regular nerve conduction studies and functional assessments help your medical team adjust treatments before irreversible damage occurs. Screening can also detect complications like foot drop, contractures, or secondary nerve compression (e.g., carpal tunnel) early. Ask your neurologist about annual assessments or when to re-test during flare cycles. Having objective data allows for fine-tuned management and can provide reassurance—or motivation to act. Don’t wait for symptoms to escalate. Staying ahead of progression is one of the most proactive things you can do.
19. Occupational Therapy for Daily Adaptation

CIDP doesn’t just affect your muscles—it affects your life. Occupational therapy helps you adapt your environment, routines, and tools to maintain independence. From custom utensils and button hooks to mobility aids and home modifications, OT ensures you don’t waste precious energy on tasks that can be simplified. Therapists also teach joint protection techniques and energy conservation strategies tailored to CIDP’s unique fatigue patterns. Occupational therapy is not just about work—it’s about how you live. Even if you’re functioning well, a proactive OT consult can help prevent strain and extend your independence.
20. Long-Term Medication Review

Many CIDP patients juggle immunosuppressants, pain medications, steroids, and more—but long-term use can bring risks. Corticosteroids may cause bone loss or blood sugar spikes, while some immunosuppressants increase infection risk. Regular medication reviews with your neurologist or pharmacist ensure your treatment is still the best option and allow for dose adjustments, transitions, or supportive therapies like bone density scans. Consider periodic reevaluation of your entire regimen—especially if you’re stable or in remission. De-prescribing where safe can reduce side effects and improve your overall quality of life. Don’t assume more meds equals better outcomes—precision is key.
Living with CIDP is a long game—one that tests your resilience, your routine, and your relationship with your own body. But as this expanded list shows, you're far from powerless. From the foods you eat to the way you move, rest, and think, every small shift counts. These 20 strategies go beyond standard treatment—they’re about reclaiming control in a world that often feels unpredictable. Whether you’re just starting your journey or navigating a difficult plateau, remember: progress isn’t always loud or linear. Sometimes, it looks like a new habit, a better night’s sleep, or a conversation that finally brings clarity. CIDP may challenge your nerves, but it doesn’t get to define your strength. So keep asking questions. Keep exploring options. Keep choosing what works for you. Because with the right tools, support, and mindset, you’re not just managing CIDP—you’re outsmarting it. One thoughtful step at a time.