9 Essential Medicine Cabinet Updates to Make Before the 2026 Flu Season
The months before flu season are the best time to make clear, practical updates to your home medicine cabinet. A small set of purposeful changes can speed recovery, reduce emergency visits, and make every family member more resilient when symptoms appear. This guide focuses on nine specific updates recommended by clinicians and public health guidance for the 2025–2026 season so you’ll be ready well before rates climb. It blends simple medical essentials with everyday wellness practices—hydration, rest, and organized care—to support both immediate symptom relief and broader recovery. Start by checking expiration dates and separating children’s supplies from adult medications. Keep current contact information for your primary clinician and local pharmacy where prescriptions can be refilled quickly if needed. If someone in your household is older, pregnant, or has chronic lung or heart disease, plan to move faster on any treatment recommendations a clinician gives. These nine updates focus on safe OTC options, monitoring tools, and care planning rather than replacing professional advice. Use them to build a medicine cabinet that serves your family’s medical needs while honoring gradual, balanced recovery practices. Where medication choices or device use are unclear, consult a healthcare provider before acting.
1. Refresh fever reducers: acetaminophen and ibuprofen
Fever reducers remain a cornerstone of at-home flu care. Most clinicians recommend having both acetaminophen (paracetamol) and an NSAID like ibuprofen available for adults and children, because different people respond differently and some symptoms improve more with one option. Keep age-appropriate formulations on hand—liquid or chewable forms for children and standard tablets for adults. Always check labels closely and follow the dosing instructions; avoid giving multiple products that contain the same active ingredient at once. Rotate out expired bottles and store medications in a cool, dry place away from direct sunlight. If someone in your household takes other prescription drugs, verify there are no interactions before combining OTC pain relievers with daily medications. For infants and young children, consult your pediatrician about exact dosing and when to seek in-person care for sustained or very high fevers. Beyond pills, simple external cooling measures—light clothing, a lukewarm sponge bath, and avoiding heavy blankets—can help comfort a feverish person while medications do their work. Use fever reducers to relieve discomfort, not just to normalize a number, and contact a clinician if the person’s condition worsens or fails to improve.
2. Add safe congestion options: saline spray and controlled decongestants

Saline nasal sprays are a gentle, widely recommended first-line tool for nasal congestion. They clear mucus without medication interactions and work for most ages, including infants when used carefully. Keep unopened bottles and single-use vials available; these are handy for quick relief and easier breathing, especially at night. For short-term symptom control, topical nasal decongestant sprays can be helpful for adults, but they should not be used for more than a few days in a row because of rebound congestion. Oral decongestants and some combination cold medicines can relieve stuffiness, yet they may raise blood pressure or interact with heart medications. If someone in your household has hypertension, heart disease, or takes monoamine oxidase inhibitors, check with a clinician or pharmacist before adding these products. Non-drug strategies—humidifiers, hot showers, and nasal irrigation—support mucus clearance and soothe inflamed passages. Consider adding a small handheld humidifier or bowl-style steam setup for the bedroom during the night when congestion is worst. Simple, low-risk options like saline often reduce the need for stronger medications and fit well with a holistic approach to breathing and rest.
3. Get a reliable digital thermometer (and know how to use it)
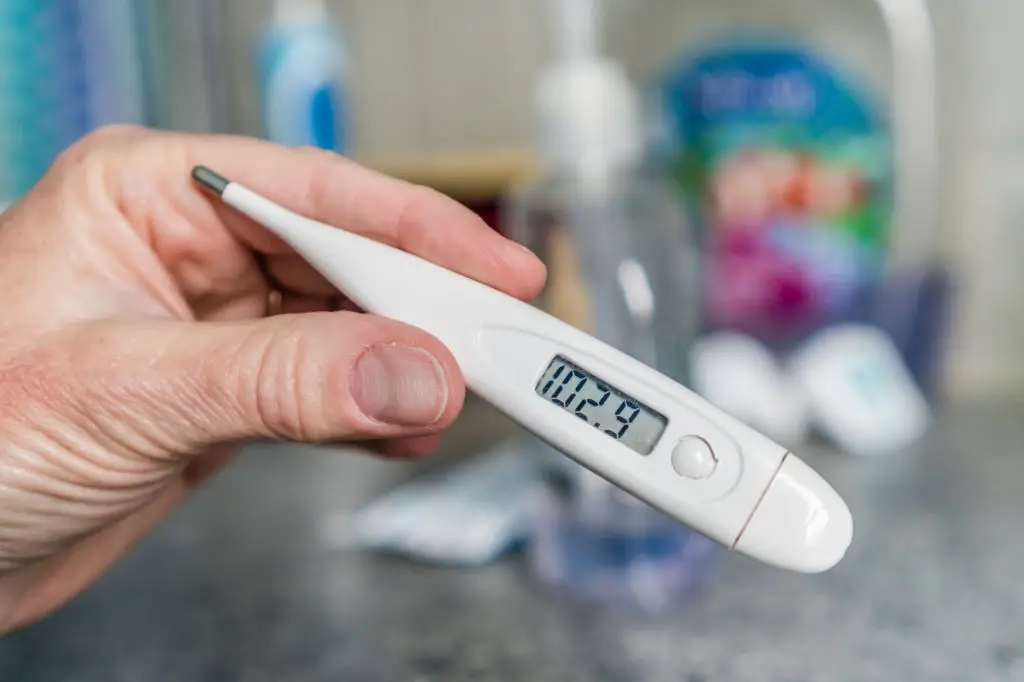
An accurate thermometer turns guesswork into clear action. A reliable digital thermometer helps you track fever trends, know when to use fever reducers, and decide if medical attention is needed. Options include oral, ear (tympanic), and temporal artery models—choose one that fits your family’s needs and learn its proper technique to avoid false readings. Keep spare batteries and clean the probe after each use, following the manufacturer’s instructions for safe hygiene. Record readings in a simple log so clinicians can see how a fever changes over time; a single temperature is less useful than the pattern across hours or days. For infants, many pediatric practices recommend specific thermometer types and thresholds for seeking care; check with your child’s clinician for guidance. In older adults or people with underlying health issues, a thermometer is also useful to support remote consultations or triage decisions. Finally, pairing the thermometer with a basic plan—when to give medication, when to call the clinician, and when to rest—makes it a practical tool rather than an anxiety trigger. Use readings to inform calm, timely decisions about care.
4. Plan for prescription antivirals: have contact and timing ready

Antiviral treatment can lessen symptom severity when started early for people at higher risk of complications. Instead of waiting to find a prescription under pressure, build a plan now: save your clinician’s after-hours contact, confirm whether telehealth visits are an option, and know which local pharmacies can fill urgent prescriptions. If a household member is older, pregnant, very young, or has chronic conditions, ask your clinician about when antiviral therapy would be recommended and what symptoms should prompt immediate contact. Timing matters—clinician guidance often emphasizes starting treatment within a specific window after symptom onset—so quick access to care is essential. Keep insurance and pharmacy details in an accessible place to speed the process. Do not try to self-prescribe or rely on expired prescriptions; always use a current prescription under clinical supervision. This planning step lowers the odds that a serious case will escalate. It also gives families peace of mind: when symptoms begin, you’ll know your next move rather than scrambling for appointments or pharmacy availability.
5. Hydration and electrolyte support: simple, effective choices

Staying hydrated is basic but powerful. Flu illness often reduces appetite and increases fluid loss through fever and sweating, so keeping simple rehydration options in the cabinet supports recovery. Stock oral rehydration solutions or electrolyte drinks for adults and children, plus easy-to-swallow options like clear broths and diluted fruit juices. For infants and toddlers, speak with a pediatrician about specific fluid choices and volumes. Plain water remains essential, but a small supply of balanced electrolyte solutions helps if someone is notably weak or not eating. Avoid high-sugar sports drinks as a primary option for children; select products labeled for rehydration or mix mild homemade solutions as instructed by a clinician. Rest and light nutrition, such as warm broths, gentle teas, and soft fruits, complement hydration to provide both fluids and easy calories needed during recovery. Keep a visual reminder—like a marked water bottle—so caregivers can track intake over 12–24 hours. Hydration is a practical step that aligns with an integrative approach to illness: it supports physiology and improves comfort.
6. Cough care: expectorants, suppressants, and throat soothers

Not all coughs are the same, and selected remedies help in different ways. Expectorants loosen mucus to ease productive coughs, while suppressants reduce the urge to cough when sleep or rest is disrupted. Choose adult or child formulations appropriately and read labels to avoid overlapping active ingredients. For children under one year, do not use honey; for those older than one, a teaspoon of honey may soothe the throat at night. Throat lozenges and warm drinks provide comfort and help control cough intensity. When cough is severe, prolonged, or accompanied by breathing difficulty, seek medical evaluation rather than relying solely on over-the-counter options. Non-drug measures—humidified air, steam inhalation, and elevated pillows at night—often reduce cough frequency and support better sleep. If household members have chronic respiratory conditions, coordinate cough care with their existing treatment plan and clinician recommendations. Thoughtful cough care eases symptoms while reducing unnecessary medication use, which supports steady recovery and clear communication with health providers.
7. Respiratory support tools: nebulizers and masks when appropriate

For people with chronic lung conditions, a pre-arranged plan for respiratory support can be critical. Nebulizers and prescribed inhaled medications are sometimes needed when symptoms worsen; if this applies to a household member, check device function, tubing, and mouthpieces now, and confirm cleaning instructions with the supplier. Masking while symptomatic can reduce spread in shared spaces; keep a small supply of disposable masks for times when stopping transmission matters. Use nebulizers only when advised by a clinician and follow strict cleaning steps to avoid contamination. For general household preparedness, a basic supply of surgical-style masks and clear instructions on wearing them correctly is a low-cost, low-risk option to protect vulnerable people at home. If you’re unsure whether a nebulizer or other device is appropriate, ask a clinician to demonstrate proper use or arrange a short telehealth check-in. These tools are supportive, not first-line replacements for clinician care, and they work best when integrated into an overall plan that includes medication, rest, and monitoring.
8. Monitoring tools beyond fever: pulse oximeter and a symptom journal
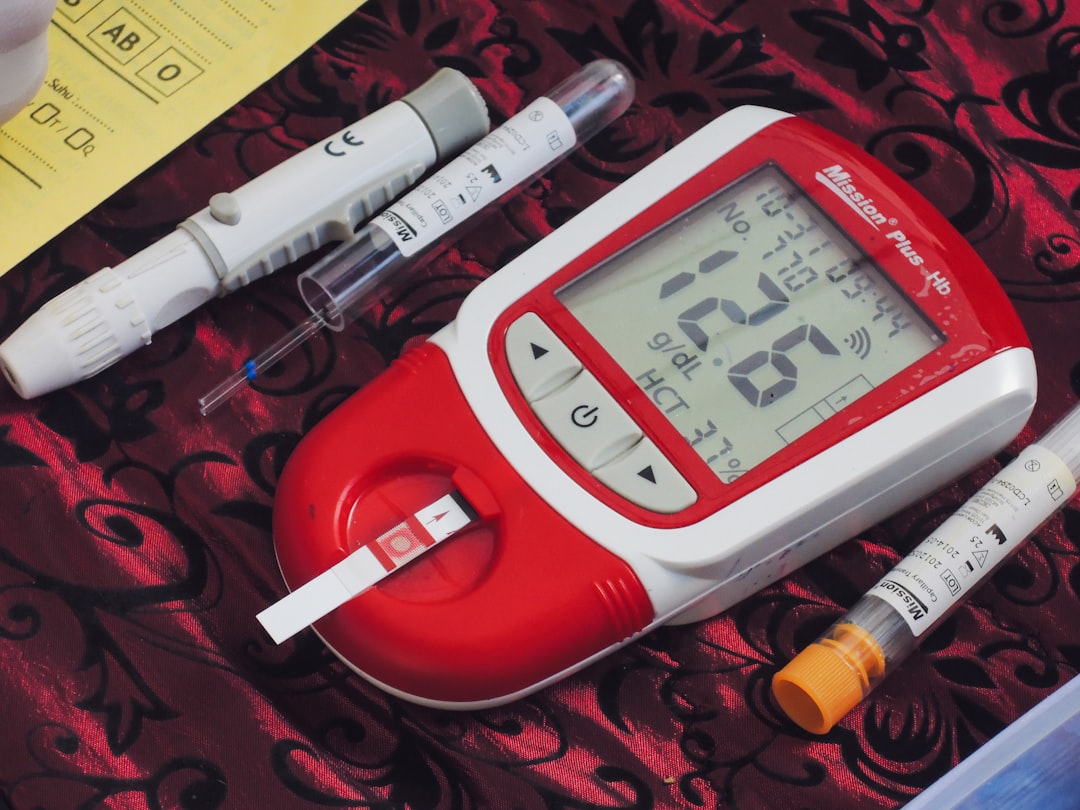
A small set of monitoring tools helps caregivers tell a clear story to clinicians. A pulse oximeter gives an objective reading of oxygen saturation and can be useful for older adults or people with lung disease; keep fresh batteries and test the device now so you know baseline values. Pair objective measures with a simple symptom journal: note onset time, peak temperatures, breathing changes, medication given, and any improvement or decline over 24–48 hours. This log speeds remote assessments and avoids miscommunication during urgent calls. Don’t fixate on single readings—look for concerning trends such as steadily falling oxygen levels, fast breathing, or progressive confusion. If you see worrying patterns, contact a clinician promptly. For many households, monitoring tools are most effective when they’re part of a plan made with a clinician in advance, including thresholds for seeking emergency care. The practice of tracking symptoms is also a mindful habit: observing changes calmly helps caregivers respond thoughtfully rather than reactively.
9. Organize, check expirations, and plan for family-specific needs

Organization reduces mistakes and speeds care when someone falls ill. Create a clear layout: child-safe area for pediatric formulations, labeled adult shelves, and a visible folder with emergency contacts, clinician phone numbers, and pharmacy details. Check expiration dates on all items and discard anything past its label date—expired products can lose effectiveness or change in safety. Make a habit of checking dates twice a year and restocking seasonally. Prepare small, portable care packs for different household members: an infant pack (with pediatric doses and clinician contact), a caregiver pack, and an older-adult pack that includes current medication lists and allergy information. Use pill organizers only for stable prescriptions; do not pre-sort short-course OTC products that require label-based dosing. Keep a printed checklist of contraindications—for example, which OTC options are not recommended for people with high blood pressure or certain heart conditions. Finally, involve everyone in the household plan so caregivers know where supplies are and how to reach help. An organized cabinet supports safer choices and faster responses when timing matters most.
Ready, steady, supported: small updates that matter

Updating your medicine cabinet before flu season is a practical act of care. The nine steps above—refreshing fever reducers, adding saline and congestion supports, ensuring accurate thermometry, planning for antivirals, maintaining hydration options, choosing appropriate cough care, preparing respiratory tools, using monitoring aids, and organizing family-specific packs—create a dependable foundation for safe, timely response. When you pair these items with early vaccination, good hand hygiene, and clear clinician connections, you reduce worry and strengthen recovery pathways for everyone in your household. Keep a simple checklist and a short symptom journal ready. Rotate stock twice a year and confirm pediatric dosing with your child’s clinician. If anyone is in a higher-risk group, move faster on clinician contact when symptoms begin. These practical steps honor a balanced approach to wellbeing: medical tools meet thoughtful caregiving, and immediate relief is matched by attention to long-term safety and recovery. Make these updates now and you’ll enter the season with steadier hands and clearer plans, ready to care for your household with confidence and calm.