Exploring the Genetics of Depression: Insights into Its Inherited Pathways
Depression, a pervasive mental health disorder, affects millions globally, yet its origins remain a complex interplay of environmental and genetic factors. Recent advances in genetic research have begun to illuminate the intricate pathways through which depression is inherited, offering new insights into its biological underpinnings. This exploration into the genetics of depression aims to decode the hereditary patterns that contribute to its onset and persistence. By examining the top ten insights into these inherited pathways, we can better understand how genetic predispositions interact with environmental triggers, ultimately paving the way for more targeted and effective interventions.
The Heritability of Depression: A Genetic Blueprint

Depression's heritability is estimated to be around 40-50%, suggesting a significant genetic component. Twin studies have been instrumental in these estimates, revealing that monozygotic twins, who share 100% of their DNA, have a higher concordance rate for depression compared to dizygotic twins. This genetic blueprint indicates that while not solely deterministic, inherited factors play a substantial role in an individual's vulnerability to depression. Understanding this heritability helps researchers identify specific genes and genetic variants that may contribute to the disorder, offering a foundation for further genetic exploration and potential therapeutic targets.
Identifying Genetic Markers: The Role of Genome-Wide Association Studies
Genome-wide association studies (GWAS) have revolutionized our understanding of the genetic basis of depression by identifying numerous genetic markers linked to the disorder. These studies scan the genomes of large populations to find variations that occur more frequently in individuals with depression. Notably, GWAS have identified loci on chromosomes that are associated with neurotransmitter regulation, stress response, and neural development. These findings underscore the complexity of depression's genetic architecture and highlight the importance of large-scale genetic studies in uncovering the myriad ways our genes can influence mental health.
Gene-Environment Interactions: The Epigenetic Influence

While genetic predisposition plays a crucial role, it is the interaction with environmental factors that often triggers the onset of depression. Epigenetics, the study of changes in gene expression without altering the DNA sequence, offers insights into how environmental factors such as stress, trauma, and lifestyle can modify genetic activity. These epigenetic changes can activate or silence genes linked to mood regulation, effectively bridging the gap between genetic vulnerability and environmental influence. Understanding these interactions is vital for developing personalized approaches to prevention and treatment, as it acknowledges the dynamic interplay between our genes and the world around us.
The Serotonin Transporter Gene: A Closer Look
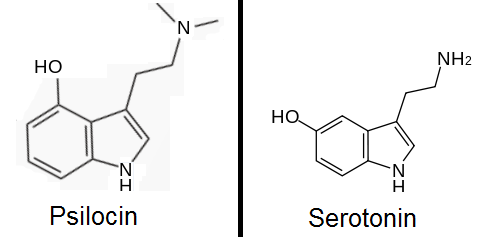
One of the most studied genetic contributors to depression is the serotonin transporter gene (SLC6A4), which regulates the reuptake of serotonin, a neurotransmitter critical for mood stabilization. Variations in this gene, particularly the presence of the short allele, have been associated with an increased risk of depression, especially in conjunction with stressful life events. This gene-environment interaction exemplifies how genetic predispositions can be exacerbated by external factors, highlighting the need for comprehensive treatment strategies that consider both biological and environmental components of depression.
Polygenic Risk Scores: Predicting Depression Susceptibility

As our understanding of depression's genetic basis deepens, polygenic risk scores (PRS) have emerged as a tool for predicting an individual's susceptibility to the disorder. PRS aggregates the effects of numerous genetic variants, providing a cumulative risk assessment. While not yet precise enough for clinical use, PRS offers a promising avenue for identifying individuals at higher risk for depression, potentially guiding early intervention efforts. As research progresses, these scores may become integral to personalized medicine, allowing for more tailored prevention and treatment strategies based on an individual's unique genetic profile.
Neuroplasticity and Genetic Influences: Adapting the Brain
Depression is often associated with changes in brain structure and function, influenced by both genetic and environmental factors. Genes involved in neuroplasticity, the brain's ability to reorganize itself, play a crucial role in this process. Variations in genes such as BDNF (brain-derived neurotrophic factor) can affect neural resilience and adaptability, potentially contributing to the onset and progression of depression. Understanding the genetic basis of neuroplasticity provides insights into how the brain can be supported and strengthened through therapeutic interventions, emphasizing the potential for recovery and adaptation even in the face of genetic predispositions.
The Role of Inflammation: Genetic Links to Immune Response

Emerging research suggests that inflammation and immune system dysregulation may contribute to depression, with genetic factors playing a role in this connection. Certain genetic variants are associated with increased inflammatory responses, which can affect brain function and mood regulation. This link between genetics, inflammation, and depression opens new avenues for treatment, such as anti-inflammatory medications and lifestyle interventions aimed at reducing systemic inflammation. By targeting these underlying biological processes, we can develop more effective strategies for managing depression at its root cause.
Gender Differences in Genetic Susceptibility

Depression is more prevalent in women than men, and genetic research is beginning to uncover potential reasons for this disparity. Hormonal differences, particularly the role of estrogen, may interact with genetic factors to influence depression risk. Studies have identified gender-specific genetic variants that affect mood regulation and stress response pathways. Understanding these gender differences is crucial for developing gender-sensitive approaches to depression treatment and prevention, ensuring that interventions are tailored to the unique genetic and hormonal landscapes of each individual.
The Future of Genetic Research in Depression: Personalized Medicine

As genetic research in depression continues to evolve, the future holds promise for personalized medicine approaches that tailor treatment to an individual's genetic makeup. Advances in genetic testing, combined with insights from epigenetics and polygenic risk scores, could lead to more precise diagnoses and targeted therapies. This personalized approach acknowledges the complexity of depression's genetic underpinnings and the need for multifaceted treatment strategies. By integrating genetic insights with clinical practice, we can improve outcomes for individuals with depression, offering hope for more effective and enduring solutions.
Bridging Genetics and Treatment
Exploring the genetics of depression provides a window into the complex interplay of hereditary and environmental factors that contribute to this pervasive disorder. By unraveling the inherited pathways of depression, we gain a deeper understanding of its biological basis, paving the way for innovative treatment approaches. The integration of genetic insights into clinical practice holds the potential to transform how we diagnose, treat, and prevent depression, moving toward a future where interventions are as individualized as the genetic factors that contribute to the disorder. This holistic understanding brings us closer to alleviating the burden of depression and enhancing the quality of life for those affected.