Guide To Treating Psoriatic Arthritis
Psoriatic arthritis is a condition in which an individual affected by psoriasis develops arthritis in their joints. Psoriasis is a skin condition where red skin patches that feature silvery scales develop on the body. A psoriasis patient may have psoriatic arthritis if they experience symptoms like pain in the soles of their feet, heel pain, swelling of the toes or fingers, deformity of the toes or fingers, and lower back pain. Psoriatic arthritis is thought to be an autoimmune disorder that occurs when the immune system inappropriately attacks tissues that make up the joints and skin. Symptoms of psoriatic arthritis usually occur when a viral infection, bacterial infection, physical trauma, or other environmental factors trigger the disease. Psoriatic arthritis diagnosis is made with the use of physical examination, x-rays, MRI scans, skin biopsy, blood tests, and joint fluid tests.
Nonsteroidal Anti-Inflammatory Drugs

Nonsteroidal anti-inflammatory drugs are medications used to help treat pain. The pain in an individual's joints that develops with psoriatic arthritis is caused by their immune processes once an inflammatory response is triggered. When the joints in an affected individual's body become inflamed, they also become swollen, red, are painful to the touch, and compress nearby sensory nerves.
Nonsteroidal anti-inflammatory drugs are specifically designed to treat pain in an individual being caused by the inflammatory process. While nonsteroidal anti-inflammatory drugs are not recommended to be used for a long duration, they can be helpful when an individual has flare-ups or episodes of symptoms related to psoriatic arthritis. Reducing the inflammation in the individual's joints by taking nonsteroidal anti-inflammatory drugs can prevent more damage to the tissues in the affected part of the body.
Immunosuppressants
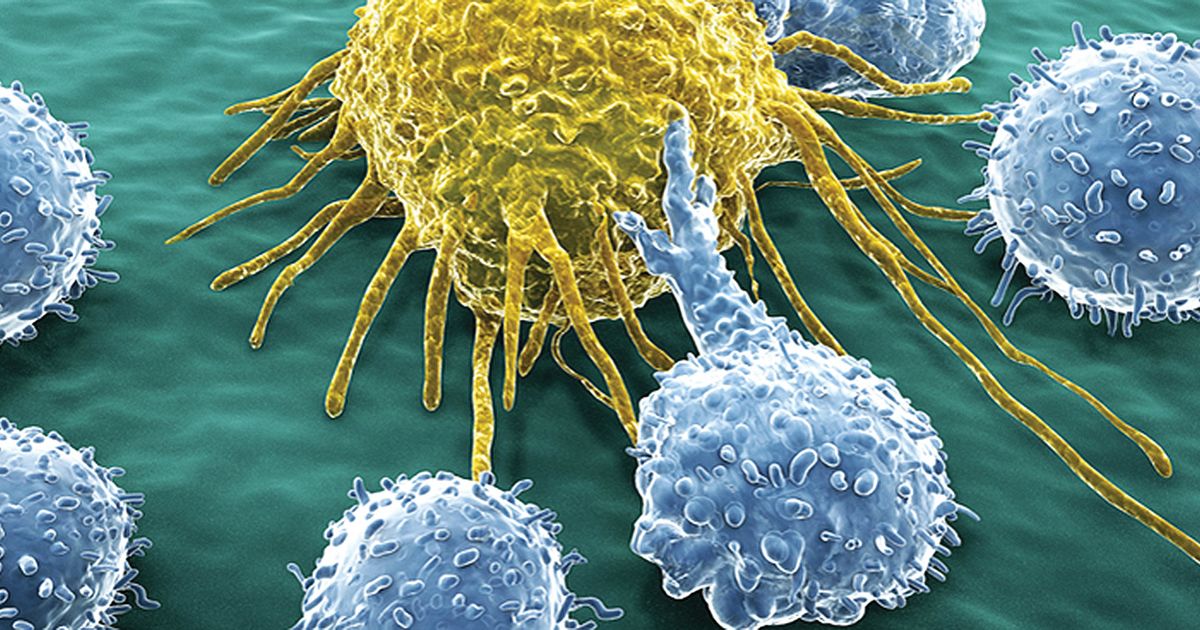
Psoriatic arthritis develops when the immune system inappropriately attacks the body's own tissues. The tissues in an affected individual that become damaged and destroyed by the immune system are those that line the joints and make up the skin. The autoimmune process that causes symptoms of psoriatic arthritis can be progressive or recurring. When other methods of treatment fail to manage the symptoms, immunosuppressants can be used to calm down the overactive immune system that is attacking the tissues of the skin and joints. The immune system is less likely to attack and cause damage to the healthy tissues in the body when its actions are toned down with medication.
Steroid Injections

A psoriatic arthritis patient may need to be treated with steroid injections when other treatment methods are not effective at managing their disorder. Corticosteroids are synthetic versions of cortisol, a hormone produced by the adrenal glands. These types of steroids decrease the action of the inflammatory processes and calm down the patient's overactive immune system. Because steroids can produce such effects, they are utilized in the treatment of a wide range of conditions related to inflammation and the action of the immune system.
Steroids can be administered orally to treat inflammation that affects multiple parts of the body simultaneously, or it can be injected into a local inflamed area. Because psoriatic arthritis is not known to produce issues in numerous organs and body systems, systemic steroids are not usually needed or used for treatment. Steroids injected directly into the affected joint(s) are preferred over systemic steroids due to fewer adverse side effects.
Joint Replacement Surgery

When an individual who has psoriatic arthritis has been unsuccessful at treating it with other methods or has a joint damaged beyond repair, they may need to undergo joint replacement surgery. This encompasses a group of surgical procedures where a patient's damaged joint is completely removed and replaced with a synthetic joint. This type of procedure is typically one of the very last treatment resorts for patients affected by any form of arthritis because it is a major procedure that carries risks, and the recovery period can take several months to several years. An individual affected by psoriatic arthritis in their knees, hips, and shoulders may need to consider the option of full joint replacement surgery if they have a reduced quality of life due to the side effects of other treatment methods or pain medication cannot control.
Physiotherapy

A psoriatic arthritis patient may need to undergo physiotherapy as part of the regimen used to treat potentially debilitating symptoms of their disorder. Psoriatic arthritis can cause inflammation-precipitated injury to the bones and other structures that make up the joints. When an individual's joints become damaged, they may lose functionality of the affected structures. Permanent damage to an affected individual's joints can also be life-changing and difficult to cope with.
Physiotherapy is a type of therapy that utilizes exercise, movement, manual therapy, advice, and education to assist patients who have damage to body structures that interfere with their everyday life. A physiotherapist can help a psoriatic arthritis patient gain functionality of their joint back when it has become injured due to the disorder. A physiotherapist can also provide tips, suggestions, advice, and education for an individual who must learn how to live with a permanently damaged joint.
