11 Options For Treating Barrett's Esophagus
Barrett’s esophagus may not cause noticeable symptoms on its own, but it carries serious implications that shouldn’t be ignored. Often developing as a complication of chronic gastroesophageal reflux disease (GERD), this condition causes the lining of the esophagus to change, resembling the tissue typically found in the intestines. While these changes are subtle and silent, the risks they bring—including an increased chance of esophageal cancer—are anything but. GERD-related symptoms like frequent heartburn, chest discomfort, and trouble swallowing often go hand-in-hand with Barrett’s esophagus, serving as red flags for potential trouble beneath the surface. Early detection and routine monitoring are crucial, especially when it comes to spotting precancerous cells that are far more treatable when caught early. To help you better understand the warning signs and prioritize your digestive health, we’ve expanded our list to 11 important symptoms and red flags associated with Barrett’s esophagus. Recognizing these signs early can lead to faster diagnosis, more effective treatment, and better outcomes overall.
1. Endoscopic Resection

Endoscopic resection is a method used to remove early-stage cancer cells and precancerous cells from the digestive tract lining. This option is an ideal alternative to traditional surgery that is sometimes used to remove precancerous and cancerous growths in the digestive tract lining. The reason for this is because endoscopic resection is considerably less invasive and less risky. This procedure is helpful for patients with Barrett's esophagus because it allows for any concerning tissues to be removed from the abnormal esophageal lining. It is imperative that these tissues are immediately extracted to stop the progression of cancerous or precancerous growths in the esophagus lining. The procedure is performed using an endoscope or a long thin flexible tube with a video camera and a light on the end of it. The surgeon inserts the endoscope into the individual's mouth, down their throat, and into their esophagus. Once located, the area of concern is carefully removed by maneuvering specialized instruments through the tube. Usually, medication is used to sedate the patient, and a numbing solution is used to ensure that they do not feel any pain or discomfort during the endoscopic resection. Most patients can return to their normal activities the next day.
2. Radiofrequency Ablation
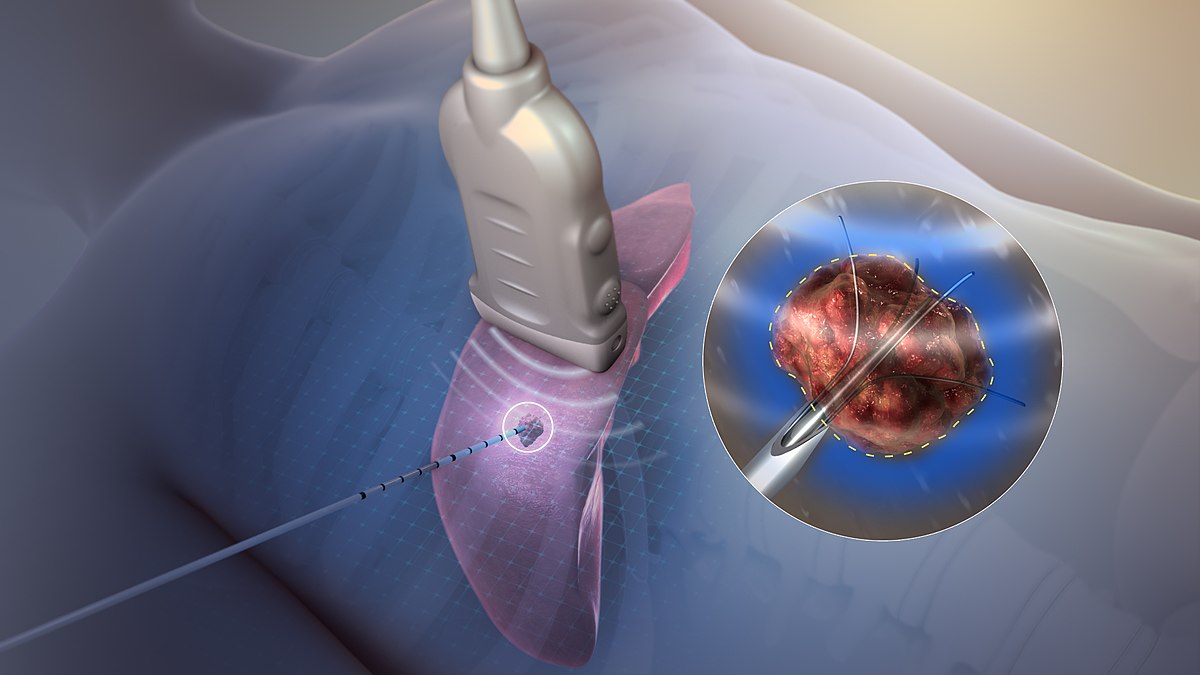
Radiofrequency ablation is a procedure used to ablate diseased or abnormal tissues in the digestive tract with the use of heat energy. Tissue ablation is performed so the abnormal tissue can be destroyed to give the body an opportunity to grow back new healthy tissues in its place. Radiofrequency ablation allows Barrett's esophagus patients to eradicate the abnormal lining of their esophagus. The procedure is carried out with the use of an endoscope similar to the one used in an endoscopic resection. However, the endoscope in radiofrequency ablation has an electrode on the end of it. The electrode is the device that will deliver heat energy directly to the abnormal tissues of the esophageal lining. Once the application of heat is administered to all of the diseased tissues, they will slough off between two and three days following the procedure. It will take the individual around six to eight weeks to regrow normal squamous cell lining in their esophagus. Depending on the extent of Barrett's esophagus, up to three separate radiofrequency ablation treatments may be required to remove all of the diseased tissues in the esophageal lining.
3. Treatment For Gastroesophageal Reflux Disease

Barrett's esophagus is a complication connected to gastroesophageal reflux disease. Because of this, treatment for GERD will help stop the progression of the abnormal esophageal lining. Usually, for mild cases of GERD, an individual will be advised to take over the counter antacids and make diet changes. If this does not help treat gastroesophageal reflux disease, medications that decrease the production of stomach acid called H-2-receptor blockers may be recommended. These medications do not work as rapidly as antacids do, though they do provide relief for a longer duration. If these measures do not help with an individual's GERD symptoms, a physician may prescribe proton pump inhibitors, which stop the production of stomach acid altogether. Another medication may be used that helps strengthen the sphincter between the stomach and esophagus. Taking this medication helps the sphincter stay closed so it cannot allow stomach acid to flow back up into the esophagus. For more advanced cases of gastroesophageal reflux disease, surgical procedures are available to treat the disease. If a patient's GERD can be managed successfully, their Barrett's esophagus will not continue to worsen.
4. Periodic Endoscopy

A critical factor in treating Barrett's esophagus is the use of a periodic endoscopy to check for cancerous and precancerous tissues. An endoscopy is a procedure utilized to examine a patient's upper digestive tract. This procedure is nonsurgical, and it is performed primarily for monitoring and diagnostic purposes. During this procedure, the individual is sedated in some form so they do not feel any discomfort or pain. The physician then passes the endoscope from the patient's mouth down into their throat, and then it is passed into the esophagus. The physician uses a monitor connected with the camera on the endoscope to inspect the tissues of the esophageal lining. If the physician sees anything concerning during the procedure, they may decide to perform a biopsy while the endoscope is already in place. The recommendation of how often a patient with Barrett's esophagus should have an endoscopy performed will depend on other risk factors such as age and familial history of cancer. Should cancerous tissue be observed in an endoscopy procedure, the patient can have it removed before it has the opportunity to spread.
5. Photodynamic Therapy

Photodynamic therapy is a nonsurgical procedure that uses medications to make abnormal cells and cancerous cells susceptible to intense light energy, like that from lasers. This technique can be used to destroy the abnormal lining of the esophagus in Barrett's esophagus patients. During photodynamic therapy, the physician will inject an infusion of a particular medication into the body through a vein. This medication causes cells to become very vulnerable to light. Within forty-eight hours of the infusion, the medication will have left the surrounding healthy tissues of the body. However, it remains in the tissue of the abnormal lining of the esophagus longer. This mechanism allows a physician to use a specialized endoscope equipped with a laser to activate the photosensitive drug that remains in the target tissues. When the light from the laser is applied, a process begins that kills the cells that form the abnormal lining. The only adverse effect of this type of therapy is the patient may remain light sensitive for thirty to ninety days following the procedure.
6. Cryotherapy

Cryotherapy is a cutting-edge treatment that uses extreme cold to destroy abnormal or precancerous cells in the esophageal lining. For individuals with Barrett’s esophagus, this technique can be a game-changer. Delivered through an endoscope, a specialized device releases either liquid nitrogen or carbon dioxide gas directly onto the diseased tissue, effectively freezing and killing the abnormal cells. The body then naturally sheds this damaged tissue and regenerates healthier cells in its place. One of the major advantages of cryotherapy is its precision—it targets problem areas without affecting surrounding healthy tissue. This treatment is especially helpful for patients who cannot tolerate more aggressive procedures, offering a gentler but highly effective approach to halting disease progression.
7. Lifestyle and Dietary Changes

While procedures and medications are essential, managing Barrett’s esophagus also requires key lifestyle and dietary changes that support long-term digestive health. Avoiding trigger foods such as spicy dishes, citrus, caffeine, and alcohol can significantly reduce GERD symptoms that contribute to Barrett’s. Eating smaller meals, maintaining a healthy weight, and staying upright after eating all help minimize acid reflux. Even simple changes like elevating the head of the bed can reduce nighttime reflux. These practical shifts, though sometimes underestimated, are a critical part of a holistic approach to slowing the progression of Barrett’s esophagus and improving quality of life.
8. Antireflux Surgery (Fundoplication)

For patients who don’t respond well to medication or prefer a long-term solution to chronic acid reflux, antireflux surgery may be recommended. The most common procedure, known as Nissen fundoplication, involves wrapping the upper part of the stomach around the lower esophagus to reinforce the lower esophageal sphincter. This helps prevent stomach acid from backing up into the esophagus, reducing the risk of further damage and progression of Barrett’s. Though more invasive than other options, surgery can offer lasting relief and may reduce or even eliminate the need for medication in some patients.
9. Surveillance Biopsies

Surveillance biopsies are a vital part of managing Barrett’s esophagus, especially for detecting early changes that may signal a progression toward cancer. During an endoscopy, small tissue samples are taken from different segments of the esophagus and examined under a microscope for dysplasia—precancerous changes in cell structure. These biopsies are often scheduled at regular intervals based on the patient’s risk level and history. While it may seem routine, this proactive monitoring strategy allows physicians to catch cellular changes at the earliest, most treatable stage, playing a crucial role in cancer prevention.
10. Esophagectomy (for Advanced Cases)

Though typically reserved for severe or advanced cases, esophagectomy—the surgical removal of part or all of the esophagus—may be necessary if Barrett’s esophagus has progressed to high-grade dysplasia or early-stage esophageal cancer. This major surgery involves reconstructing the digestive tract, usually by pulling up a portion of the stomach to replace the removed section of the esophagus. While it's a more aggressive intervention, esophagectomy can be lifesaving and potentially curative when performed at the right stage. It's considered when other therapies are unlikely to be effective or when cancer is already present.
11. Genetic and Molecular Testing

Emerging research has led to the use of genetic and molecular testing to assess cancer risk in patients with Barrett’s esophagus. These advanced tests analyze specific biomarkers in esophageal tissue samples to detect early signs of dysplasia or malignant transformation—sometimes before traditional biopsy methods can. For patients with a family history of esophageal cancer or those showing signs of rapid progression, these tests can provide a clearer picture of risk and help guide more personalized treatment plans. While not yet standard across all practices, they represent an exciting frontier in early detection and individualized care.
Taking Charge of Barrett’s Esophagus Before It Takes Hold

Barrett’s esophagus may not shout for attention, but its silent progression can lead to serious consequences if left unchecked. The good news? With a growing arsenal of treatment options—from advanced procedures like radiofrequency ablation and cryotherapy to lifestyle changes and regular surveillance—you have more control than ever. Early detection is your strongest defense, and recognizing the warning signs linked to GERD can make all the difference. Whether it’s through cutting-edge therapies or everyday diet adjustments, each proactive step helps slow disease progression and reduces the risk of esophageal cancer. By partnering with your healthcare provider and staying informed, you can transform a potentially dangerous diagnosis into a manageable condition. Don’t wait for symptoms to escalate—monitor your health, ask questions, and take action. Because when it comes to Barrett’s esophagus, awareness isn’t just power—it’s protection.
