15 Common Causes And Risk Factors For Septic Arthritis
Septic arthritis isn’t just painful—it’s potentially dangerous. This serious joint infection can strike when bacteria or other germs enter the bloodstream and settle into a vulnerable joint, or when an injury gives them direct access. While anyone can be affected, infants, older adults, and individuals with compromised immunity are especially at risk. The condition most often targets the knees but can also inflame hips, shoulders, and other joints. If left untreated, septic arthritis can rapidly destroy cartilage and bone, leading to permanent damage. That’s why early diagnosis and treatment—typically involving antibiotics and joint drainage—are critical. But how does this condition take hold in the first place? The answer often lies in overlooked triggers and subtle health factors. We’ve expanded our list to include 15 Common Causes and Risk Factors for Septic Arthritis—from chronic conditions and surgical risks to lifestyle habits and infections. Understanding them could be the key to prevention—and protection.
1. Various Types Of Infections

Septic arthritis can develop because of various types of infections, including fungal, viral, and bacterial infections. Staph infections, a common bacterial infection, are most often cited as the cause. These infections are unusually common because the bacteria can live and survive on both healthy and infected skin, so individuals are at risk of developing an infection regardless of their overall health. Usually, septic arthritis develops when infections from elsewhere in the body spread via the bloodstream, lodging in the joint. These might include common infections like urinary tract infections or skin infections. Joints are lined by a material called synovium, which isn't designed to protect itself against infections. Since the joint is so susceptible to infection, the body responds with an inflammatory and strong immune response that contributes to the joint damage through increased pressure and swelling.
2. Weakened Immune System
Individuals with a weakened immune system have a higher chance of developing septic arthritis. Patients with kidney problems, liver problems, diabetes, immune-weakening viruses, and individuals taking immunosuppressants are in this increased risk category. Joints are already susceptible to germs and infection even in cases where the individual is healthy. When the joint becomes infected and the immune system can't destroy the infection, the condition just continues to worsen. The infection eats away at the joint and surrounding tissues. Joint cavities are small and enclosed, so infections can cause a huge amount of damage in very little time. While immune responses can contribute to joint damage, individuals with weakened immune systems will have infections that spread more rapidly. Delayed treatment can cause permanent joint damage and degeneration.
3. Joint Trauma

In less common cases, a surgery, drug injection, or puncture wound around or inside the joint can allow germs to enter the joint cavity. It's unusual for individuals to experience injuries that cause such direct access to the joint, which is why this method of infection is much rarer than infection from the bloodstream. Experiencing joint trauma puts individuals at a higher risk of developing septic arthritis, even if the wound doesn't appear to be on the joint itself. While deep punctures are the most common methods of infection, it's possible shallow wounds might also lead to germ transmission. The risk also increases if the cause of the injury was unsanitary. For example, animal bites or punctures from dirty needles can transmit germs much more easily than clean cuts. If an individual is injured around or on their joint, it's important for them to clean and bandage the wound as soon as possible. They should also monitor it closely for signs of infection.
4. Rheumatoid Arthritis

Rheumatoid arthritis is a condition where the immune system creates antibodies that attack joint tissue. Normally, antibodies are supposed to attack viruses, infections, and other invasive substances. The mistaken system-attacking antibodies make this condition an autoimmune disease, a class of illnesses caused by immune system malfunctions. Typical treatments for rheumatoid arthritis include immune-suppressing medications. Like with patients whose immune systems are weakened due to illness, this can cause the infection to progress and cause more damage. It's also difficult to get a septic arthritis diagnosis when an individual has rheumatoid arthritis, because many of the symptoms are very similar. Some rheumatoid arthritis patients don't realize their condition is something other than the usual pain, swelling, and inflammation until it's too late. For this reason, it's important for patients with rheumatoid arthritis to be aware of the risks of septic arthritis. They should be informed of the potential causes and warning signs so they can seek prompt medical treatment.
5. Osteoarthritis
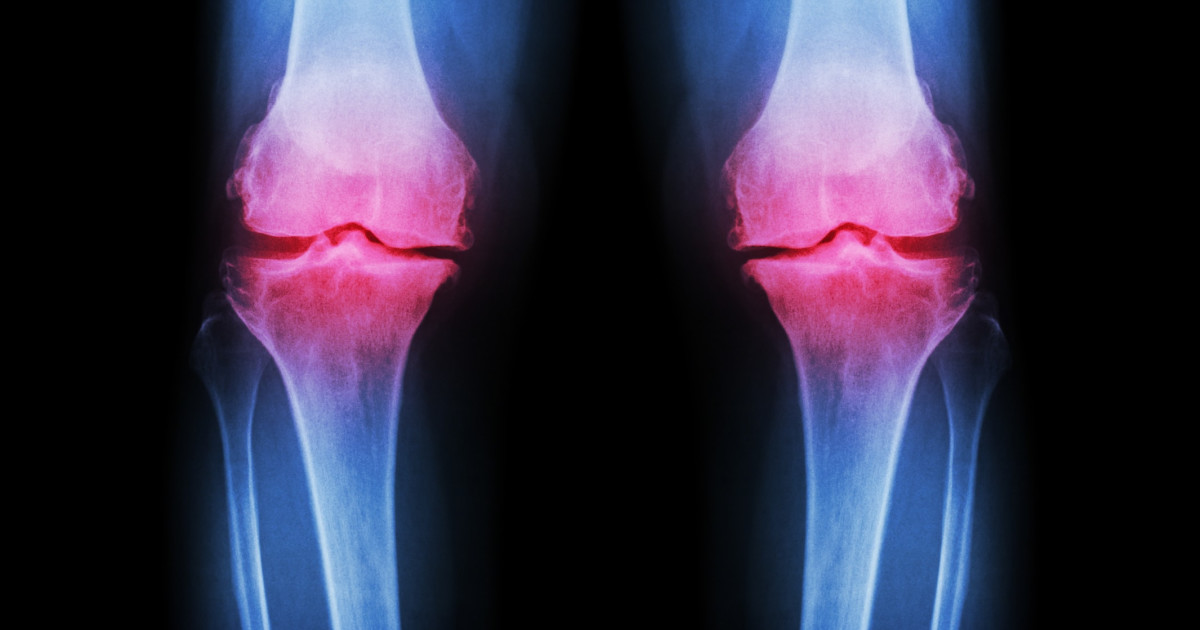
Osteoarthritis is just one of several conditions that can increase an individual's risk of developing septic arthritis. When a patient already has problems with their joints, the joints are more susceptible to infection due to weakness and prior damage. Chronic joint conditions like osteoarthritis, lupus, and gout are often seen alongside septic arthritis cases. Osteoarthritis most commonly affects the joints in an individual's spine, hips, hands, and knees, though it is possible for any joint to be affected. Typically, symptoms include joint stiffness, pain, and tenderness, as well as a grating sensation when the affected joint is used, a loss of flexibility in the joint, as well as bone spurs. It is crucial for osteoarthritis patients to receive appropriate and prompt treatment in order to mitigate the potential for septic arthritis to develop.
6. Recent Joint Surgery

Undergoing joint surgery, such as a hip or knee replacement, significantly increases the risk of septic arthritis. Despite sterile environments and antibiotics, bacteria can still be introduced during surgery or in the recovery period. Prosthetic joints, in particular, are more vulnerable to infection because bacteria can adhere to artificial surfaces and evade the immune system. Once infected, artificial joints often require complex treatments, including surgical removal. Early post-op symptoms like joint pain, swelling, and warmth should never be dismissed. Patients recovering from joint surgeries must monitor for signs of infection and follow post-operative care strictly.
7. Skin Conditions Near Joints

Chronic skin conditions such as eczema, psoriasis, or infected wounds near joints can increase the likelihood of bacteria entering the joint space. When skin integrity is compromised, especially near the elbows, knees, or fingers, pathogens have easier access to internal tissues. Individuals who scratch or pick at these areas can unintentionally drive bacteria deeper, increasing the risk of septic arthritis. Even minor abrasions can act as entry points if not cleaned properly. Maintaining skin health, treating rashes promptly, and preventing infection around joints are crucial preventative steps, especially for those with preexisting joint disorders.
8. Intravenous Drug Use

Individuals who use intravenous drugs face a heightened risk of septic arthritis, particularly when needles are shared or used in non-sterile conditions. Bacteria can enter the bloodstream directly through contaminated injections and travel to the joints. Additionally, repeated injections may lead to local infections or skin abscesses that further spread. The knees, hips, and shoulders are especially vulnerable. Because symptoms can be mistaken for general body aches or withdrawal pain, infections may go unnoticed until significant damage has occurred. Education, harm-reduction strategies, and timely access to healthcare are critical for prevention.
9. Age-Related Vulnerability

Both the very young and the elderly are disproportionately affected by septic arthritis. Infants may contract it due to underdeveloped immune systems, often following infections like umbilical stump infections or respiratory illnesses. In older adults, declining immunity, reduced circulation, and existing joint degeneration make infections more likely and more damaging. Moreover, symptoms in seniors—such as fatigue or confusion—may be misattributed to other conditions, delaying diagnosis. This age-based vulnerability underscores the need for close observation and swift medical evaluation when new joint pain or swelling appears in these populations.
10. Hemodialysis Treatment

Patients undergoing hemodialysis are at increased risk due to repeated vascular access and a compromised immune state. Each dialysis session introduces the potential for bacteria to enter the bloodstream, especially if proper hygiene isn't maintained. Furthermore, individuals with end-stage kidney disease often experience chronic inflammation and are more susceptible to systemic infections. Once bacteria reach the bloodstream, they can easily localize in the joints. For dialysis patients, vigilant infection control—both during treatment and at home—is essential to reduce the risk of life-threatening complications like septic arthritis.
11. Diabetes Mellitus

Diabetes impairs the immune response and slows the body’s ability to fight infections—making even minor wounds potentially dangerous. Elevated blood sugar also creates an environment where bacteria thrive. Diabetics often experience joint problems like Charcot joint or osteoarthritis, which adds structural vulnerability. These factors combined make septic arthritis a serious risk. Foot ulcers or skin breaks can act as bacterial entry points, especially in patients with neuropathy who may not feel early symptoms. Regular skin inspections, blood sugar control, and rapid infection treatment are critical for prevention.
12. Use of Corticosteroids

Chronic or high-dose corticosteroid use—whether taken orally or injected directly into joints—can suppress the immune system, leaving patients more susceptible to infection. Corticosteroids may also mask the inflammation and pain typically associated with septic arthritis, delaying diagnosis. Joint injections, especially when repeated, carry a small but real risk of introducing bacteria if not administered under strictly sterile conditions. Physicians typically balance the benefits of inflammation control with the potential infection risks, especially in patients with existing joint damage or immune compromise.
13. Gonorrhea and Sexually Transmitted Infections (STIs)

Certain STIs—especially gonorrhea—can spread to the joints, leading to a form of septic arthritis known as disseminated gonococcal infection (DGI). It’s more common in sexually active young adults and women. Symptoms often begin subtly, with joint pain and skin rashes, and may be mistaken for other conditions. Untreated gonorrhea can enter the bloodstream and settle in one or multiple joints. Prompt diagnosis and antibiotic treatment are crucial. Preventing transmission through safe sex practices and regular screening is a key step in reducing this often-overlooked cause.
14. Immunosuppressive Therapies

Patients receiving immunosuppressive therapies—such as chemotherapy, TNF inhibitors, or biologics for autoimmune conditions—are more prone to septic arthritis. These drugs, while essential for managing diseases like lupus, rheumatoid arthritis, or Crohn’s, reduce the body’s natural ability to ward off infections. As a result, even minor bacterial invasions can become serious joint infections. Patients should be educated about infection risks before starting such treatments and should be encouraged to report unexplained joint pain or swelling promptly. Preventive vaccinations and routine monitoring help mitigate the danger.
15. Recent Travel or Animal Exposure

Exposure to rare bacteria or parasites during international travel or close contact with animals can also trigger septic arthritis. Bacteria like Brucella (from livestock), Pasteurella (from animal bites), or even Mycobacterium tuberculosis can infect joints in vulnerable individuals. Travel to regions with poor sanitation or handling raw animal products increases risk. Unlike common bacterial infections, these may cause slower-developing but chronic joint inflammation. Doctors may overlook the link unless travel or exposure history is shared—so keeping track of unusual activities is vital for early diagnosis.
Septic arthritis may strike fast, but knowledge strikes first. Understanding the wide range of causes and risk factors—from existing joint conditions and recent surgeries to lifestyle habits and hidden infections—can be the difference between early intervention and long-term damage. This isn’t just about joint pain—it’s about preserving mobility, independence, and quality of life. While the condition can be serious, it’s also treatable—especially when caught early. By staying alert to the risks and knowing what symptoms to watch for, individuals and caregivers can act swiftly and effectively. Whether you’re managing chronic arthritis, recovering from surgery, or supporting someone with a weakened immune system, awareness is your best defense. Now that we've uncovered 15 common causes and risk factors for septic arthritis, use this information not just to stay informed—but to stay ahead. Because when it comes to joint health, prevention isn’t just possible—it’s powerful.
