Causes And Complications Of Wilson's Disease
Wilson's disease, also known as hepatolenticular degeneration and progressive lenticular degeneration, is a genetic condition inherited as a result of an autosomal recessive trait. This progressive condition causes the body to accumulate too much copper in the liver, eyes, brain, and other organs, and treatment is needed to prevent long-term disability and early death. Genetic testing can be performed to diagnose Wilson's disease, and the clinician will also check for signs of the liver and eye damage associated with the disorder. Most patients with Wilson's disease are diagnosed in their teens or early twenties. Treatment generally includes a combination of chelating agents, zinc salts, and tetrathiomolybdate in an attempt to reduce the patient's copper levels to a nontoxic range.
Some of the major causes and potential complications of Wilson's disease are described below.
Autosomal Recessive Genetics

Autosomal recessive genetics refers to the particular inheritance pattern associated with Wilson's disease. The disease is an autosomal recessive disorder, and scientists have discovered it is caused by mutations to the ATP7B gene. Currently, more than three hundred mutations to this gene have been identified. Wilson's disease is inherited when the patient receives two copies of the mutated gene for this condition, one from each of their parents. If the patient only receives one copy of the mutated gene associated with Wilson's disease they will be a carrier of the disease but will not have symptoms. If both parents are carriers of Wilson's disease, there is a twenty-five percent chance their child will be born with the disease and a twenty-five percent chance they will be born without it. There is a fifty percent chance their child will be born as a carrier of the disease. Genetic counselors can help parents who are carriers of Wilson's disease learn more about their chances of passing this condition to their children.
Keep reading to reveal the complications linked to Wilson's disease now.
Cirrhosis Of The Liver

Cirrhosis of the liver is one of the potential complications that may develop from Wilson's disease. As the patient's body attempts to clear the buildup of excess copper from the liver, scar tissue is formed in the area, compromising the normal liver function. In the early stages of cirrhosis, patients may be asymptomatic, with symptoms appearing only in the most advanced stages. Late-stage symptoms of cirrhosis include jaundice, itchy skin, fatigue, swelling in the legs, and loss of appetite. Some patients may also have redness on the palms of the hands and fluid accumulation in the abdomen. For patients with Wilson's disease, liver abnormalities can begin as early as six years of age. Therefore, even young patients may need to have regular blood tests to check liver function, and ultrasounds, MRI scans, and liver biopsies can help assess the severity of liver damage and cirrhosis. Treatment for cirrhosis of the liver focuses on the underlying cause, and medications to reduce copper levels can sometimes improve liver function and prevent liver scarring for patients with Wilson's disease. Advanced cirrhosis can be life-threatening, and patients at this stage may need a liver transplant.
Uncover more Wilson's disease complications now.
Kidney Stones
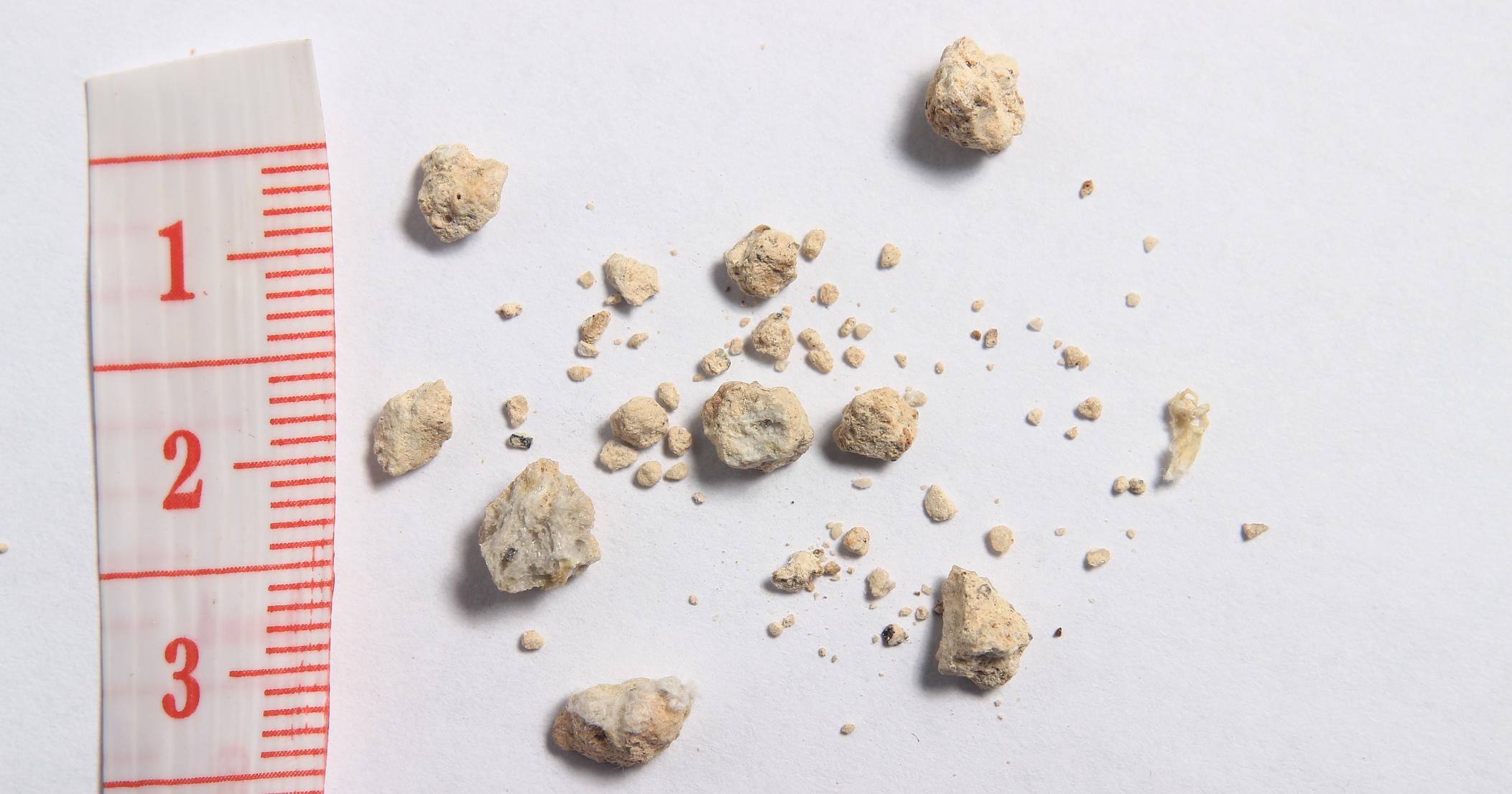
Patients with Wilson's disease have an increased risk of developing kidney stones, which are formed from tiny deposits of the salts and minerals that are normally filtered by the kidneys. While the stones typically cause no permanent damage, they can cause considerable pain. Possible symptoms include pain while urinating, an increase in urinary frequency or urgency, and cloudy urine. Patients could experience severe pain in the back or side that fluctuates in intensity, and it might radiate to the groin or lower abdomen. The patient's urine may also be bloody. To diagnose kidney stones, doctors may perform blood tests and a twenty-four-hour urine test. Ultrasounds, CT scans, and other imaging studies can be used to detect small stones. Due to their increased risk for kidney stones, it is recommended that patients with Wilson's disease have an annual x-ray to check for any stones. If small stones are found, these can often be passed with the help of pain relievers, alpha blockers, and plenty of fluids. Larger stones can be removed through extracorporeal shock wave lithotripsy and other surgical interventions.
Learn more about the complications associated with Wilson's disease now.
Hemolysis

Hemolysis is characterized by the abnormal destruction of red blood cells, and it is a potential complication for patients with Wilson's disease. In healthy individuals, red blood cells generally have a lifespan of around 120 days. Hemolysis greatly reduces this lifespan, and it can result in hemolytic anemia. This condition causes patients to feel fatigued, and they may also have an increased heart rate and an enlarged spleen or liver. Patients may feel weak, and they could become dizzy or confused. Blood tests can determine the extent of a patient's hemolysis, and treatment options include transfusions of red blood cells, infusions of immunoglobulin, and corticosteroids to suppress the immune system. Some patients may require surgery to remove the spleen.
Get the details on additional complications of Wilson's disease now.
Neurological Issues

Patients with Wilson's disease may experience a variety of neurological issues. For example, lack of coordination, gait abnormalities, tremors, and slurred speech could occur. Some individuals might experience involuntary muscle movements or twitching, and speech difficulties have been observed. For some patients, neurological issues could be accompanied by psychological changes such as depression, irritability, mood swings, and changes in personality. Bipolar disorder and episodes of psychosis may develop. These neurological and psychological changes typically improve or resolve with appropriate treatment for Wilson's disease, although some patients may have lingering neurological difficulties even with treatment. To assess neurological issues, clinicians will check the patient's gross and fine motor skills and check for any signs of involuntary muscle movements. If present, psychological changes can be addressed with a mental health specialist. In addition to medications for Wilson's disease, patients may benefit from other medicines that could reduce tremors and muscle twitching. Medications for mental health concerns might be useful as well.
