Guide To The Causes And Risk Factors Of Periventricular Leukomalacia
Periventricular leukomalacia is a type of injury incurred to the brain of infants born prematurely or at a low weight. Periventricular leukomalacia occurs when the delicate brain tissues that sit around the ventricles die due to one or more acute mechanisms. This delicate brain tissue is called white matter, and white matter is the tissue responsible for the production of myelin, a fatty substance that covers and protects the nerve axons, allowing impulses to travel from one nerve to the next in a smooth manner.
Individuals affected by periventricular leukomalacia have nerves that cannot conduct electrical signals properly because they are unprotected and uninsulated. This malfunction causes problems with the nervous system and healthy development. There are several possible causes and risk factors of periventricular leukomalacia.
Hypoxia Or Ischemia
A periventricular leukomalacia patient may have experienced hypoxia and ischemia. Brain ischemia refers to a condition where there is not enough blood flowing to the brain to give the brain tissues an adequate amount of oxygen. Hypoxia of the brain is a condition where there is not enough oxygen reaching the tissues in the brain. Ischemia always causes hypoxia in the affected tissues, but hypoxia of the tissues can be caused by mechanisms other than ischemia.
Any mechanism that causes an infant to have reduced blood flow to the brain can cause periventricular leukomalacia, such as having the umbilical cord around the neck during birth, pressure compression to the blood vessels supplying the infant's brain, and blood clots lodged in the vessels supplying the infant's brain with blood. Any mechanism that causes an infant to have poor oxygen saturation in the blood flowing to their brain can cause the injury of periventricular leukomalacia, such as maternal anemia, underdeveloped lungs, neonatal congenital heart disease, neonatal cardiovascular collapse, shoulder dystocia, and placental insufficiency.
Hypotension

An unborn child who's mother experiences hypotension before or during the birthing process may develop periventricular leukomalacia as a complication of the maternal condition. Hypotension is a blood pressure of less than 90/60. Low blood pressure throughout an individual's pregnancy causes reduced blood flow to the unborn child, which results in a reduced amount of oxygen and nutrient delivery. Ischemia-precipitated periventricular leukomalacia can occur in unborn children when the mother experiences hypotension throughout their pregnancy. Hypotension is also a common occurrence when a pregnant woman is in the process of giving birth, which may also cause an unborn child to experience a brain injury.
Most cases of maternal hypotension during labor are related to the use of spinal anesthesia and the position of the mother when the spinal anesthesia is administered. Hypotension-precipitated periventricular leukomalacia can also occur in the affected individual following their birth. Hypotension is most common in neonates who have a heart infection, sepsis, loss of blood, problems with adrenal glands, patent ductus arteriosus, and abnormal heartbeats. Hypotension can also be caused in a neonate when a ventilator is required because of increased pressure in the chest.
Intraventricular Hemorrhage
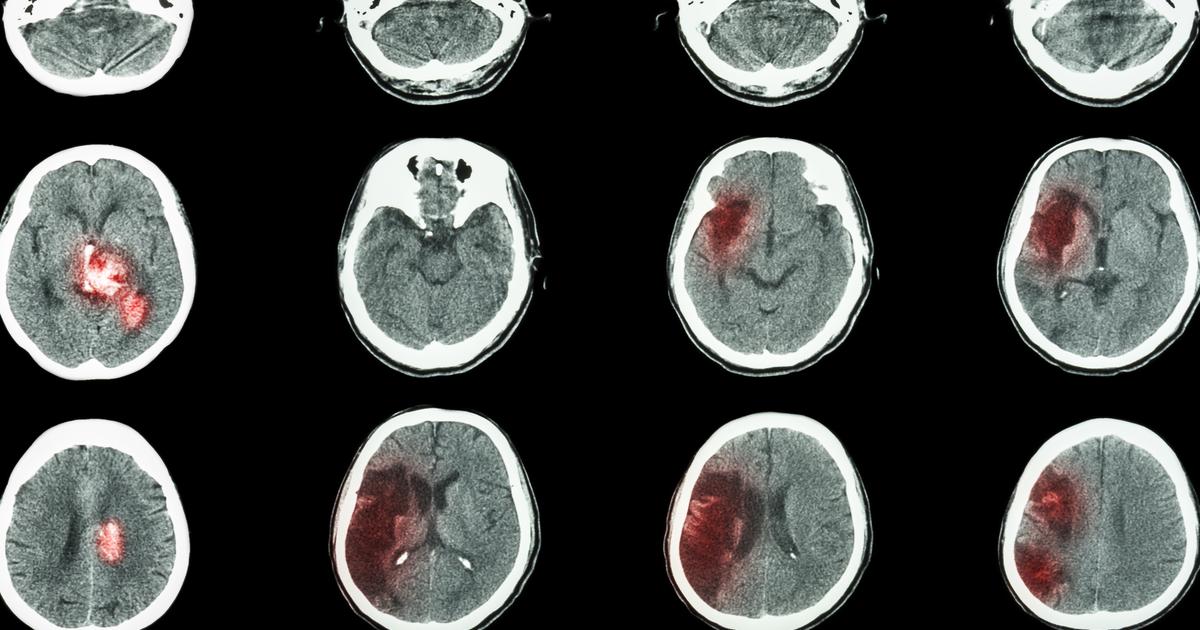
An infant or unborn child affected by an intraventricular hemorrhage may develop periventricular leukomalacia as a complication of their emergent medical event. Intraventricular hemorrhage is a term used to describe when an individual experiences a bleed inside or around their brain ventricles. Brain ventricles are the spaces in an individual's brain filled with cerebrospinal fluid. Periventricular leukomalacia occurs when the white matter in the spaces between the individual's ventricles becomes damaged and can no longer produce the protective myelin sheath that covers the nerves.
An intraventricular hemorrhage causes blood to flow into these spaces that put excessive pressure on the cells that make up the white matter, which causes them to become damaged beyond repair and die. Intraventricular hemorrhage-precipitated periventricular leukomalacia is most common in babies born prematurely. The exact reason for this is not clear, but it is thought the increased fragility of a premature infant's blood vessels leads to their increased risk of intraventricular hemorrhage.
Infection In The Uterus

A periventricular leukomalacia patient may have been affected by an infection in the uterus before being born. The mechanism of how a maternal infection that crosses into uterus causes brain injury that leads to periventricular leukomalacia is not associated with immediate changes in the flow of blood to the unborn child's brain, unlike most of the other causes of the brain injury. Instead, it is thought the infection makes its way into the amniotic membranes around the unborn child and releases harmful toxins into the fluids. The harmful toxins released by the infection-causing pathogen cause the blood vessels in the unborn child's brain to develop abnormally.
Abnormally formed blood vessels in the brain can cause problems later in the pregnancy and during the birth of the child. Certain infections that cross the uterus into the membranes around the unborn child are also known to produce inflammation in the umbilical cord and membranes, which increases the chance of periventricular leukomalacia. This increased risk is attributed to swelling and how it can interfere with the normal flow of blood. Maternal sepsis can be transferred to the blood of an unborn child, which has direct effects on the white matter in the brain, which may also cause periventricular leukomalacia.
Premature Infants

The risk of experiencing periventricular leukomalacia is greatest in premature infants. An unborn child is at the highest risk of this type of brain injury when they are within the gestational ages of twenty-six weeks to thirty-four weeks. Periventricular leukomalacia occurs most often in infants born before the gestational age of thirty-two weeks and those with a birth weight of under 3.3 pounds. A positive correlation between the occurrence of periventricular leukomalacia and premature infants that require mechanical ventilation upon birth has also been made.
Premature infants have very fragile white matter in their brains that can be more easily damaged by factors like trauma, infections, and stress. In full-term infants, most of the causes of periventricular leukomalacia can be prevented or mediated if the correct and prompt medical actions are taken. However, prevention and resolution may not always be possible in infants born prematurely because they are underdeveloped, and their tissues are more fragile than those of full-term infants.
