Causes And Risk Factors Of Toxoplasmosis
Toxoplasmosis is a parasitic infection that can develop through ingestion of the T. gondii parasite. Most patients who have toxoplasmosis are asymptomatic, and if symptoms do appear, they generally consist of headache, sore throat, fever, swollen lymph nodes, and muscle aches. The symptoms could persist for at least four weeks, and they frequently resolve on their own without treatment. For patients with weakened immune systems, toxoplasmosis can be especially dangerous, and it may lead to complications such as infections of the lungs, brain, or eyes.
Patients with these complications might experience blurred vision, shortness of breath, and seizures, and comas have occurred. To diagnose toxoplasmosis, doctors can perform blood tests. If treatment is needed, specialists typically use medications such as pyrimethamine or sulfadiazine. Pregnant women with toxoplasmosis might also need to take clindamycin and leucovorin.
Consuming Contaminated Water Or Food

Patients may unknowingly ingest the parasite that causes toxoplasmosis by consuming contaminated water or food. In the United States, it is very rare for treated water to contain T. gondii. Individuals traveling to countries where water quality may be an issue should consider buying water filtration devices and chemical disinfectants to take with them, and it may be advisable to only drink bottled water in certain locations.
In terms of food, lamb, venison, and pork are much more likely to be contaminated with T. gondii than other meats, and patients need to ensure all meat is fully cooked before eating. Individuals who have weakened immune systems, including cancer patients, may wish to avoid eating these kinds of meat while receiving treatment. Any cutting boards, utensils, and other items that have come into contact with raw meat should be properly cleaned in hot, soapy water to prevent contamination with the T. gondii parasite.
Infected Organ Transplant

Although very rare, patients receiving an organ transplant could contract toxoplasmosis if they are given an infected organ. Patients who have both solid organ transplants and stem cell transplants are at risk. A patient's risk of contracting toxoplasmosis from an organ transplant is related to the overall prevalence of the infection in the location where the organ was donated. For example, rates of toxoplasmosis in the general population are high in Europe, and the incidence of infected organ transplants is also higher there. Certain types of transplants, including heart transplants, are associated with an increased risk of infection with toxoplasmosis. This is because the heart is a recognized site of encystation of the T. gondii parasite.
Patients who develop toxoplasmosis following a transplant will typically develop symptoms within two weeks to three months of the transplant date. To reduce the risk of getting toxoplasmosis from an organ transplant, organ donors and recipients are given a range of blood tests that can identify individuals at high risk for this infection. High-risk patients are normally given a prescription for co-trimoxazole to reduce their risk. Individuals having a transplant should ask their healthcare team about their risk of toxoplasmosis and steps they can take to reduce this.
Infected Blood In A Transfusion

Receiving infected blood in a transfusion is a rare cause of toxoplasmosis. A 2014 article in the Iranian Journal of Parasitology determined the prevalence of toxoplasmosis in blood products was 23.6 percent, and a 2016 article reported the global prevalence of toxoplasmosis in donated blood is thirty-three percent. To protect the recipients of blood products, individuals who have had toxoplasmosis are required to refrain from donating blood until at least six months after they have made a complete recovery. Since blood donations are not currently screened for toxoplasmosis, donors who have had this infection need to inform staff they have had toxoplasmosis before donating.
If they have recovered and are approved to donate, a note will be placed on their donation so it will not be given to patients with weakened immune systems. Individuals who have received a blood transfusion should carefully monitor their health for any changes, particularly for the development of the flu-like symptoms associated with toxoplasmosis. If these symptoms occur, recipients should see a doctor as soon as possible, and they may wish to be screened for toxoplasmosis.
Contact With Cat Feces

Currently, cats are the only known hosts of the T. gondii parasite. This means the parasite's eggs sexually reproduce in cats, and the eggs exit the cat's body through feces. The parasite is found in both wild and domestic cats, and cats that hunt or eat raw meat are more likely to be infected. Contact with cat feces is most likely to occur while cleaning out a cat's litter box, and this is a particularly common method of toxoplasmosis infection.
After cleaning a litter box, individuals should wash their hands thoroughly and use an alcohol-based hand sanitizer. To minimize contact with cat feces, it may be worthwhile to invest in a litter box that includes an automatic cleaning feature. Patients might also come into contact with cat feces while gardening in the soil or while touching cat bedding or toys that could be contaminated with fecal matter.
Chemotherapy
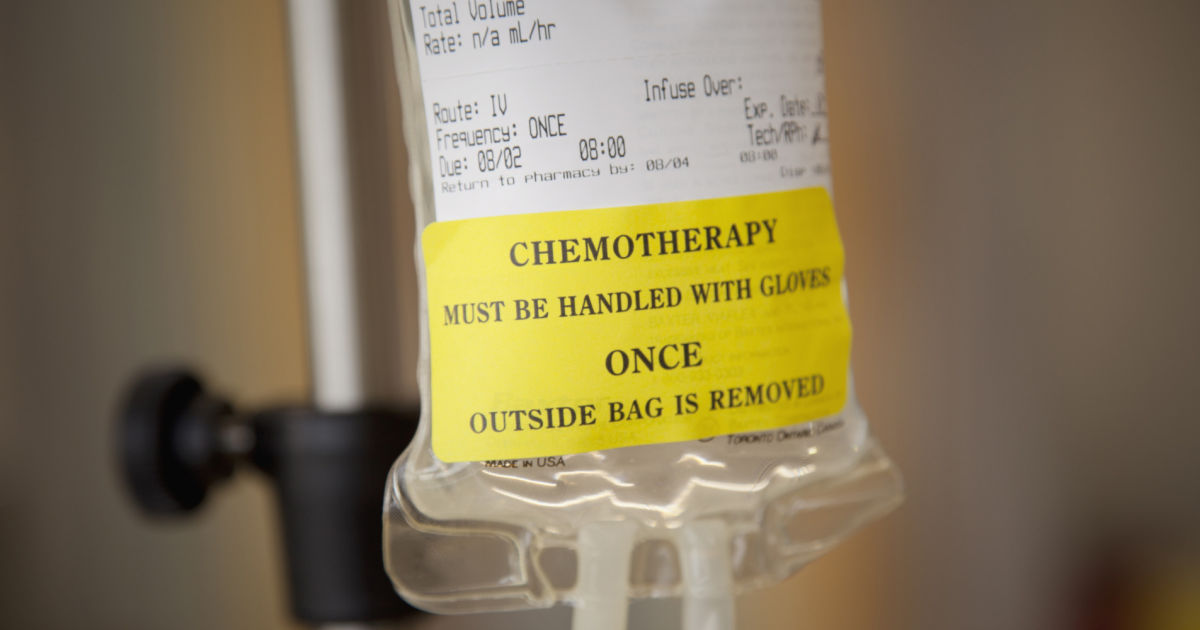
Chemotherapy weakens the immune system, and this makes patients more vulnerable to infection with toxoplasmosis. Individuals receiving chemotherapy should not clean out a cat's litter box, and they should be especially careful to wash their hands after petting or feeding cats. While on chemotherapy, patients may need to ask a family member or friend for help in caring for a cat. A doctor should be contacted promptly if any flu-like symptoms develop, and patients should inform their healthcare team they have spent time around cats. Depending on the patient's symptoms, doctors may recommend the patient be tested for toxoplasmosis. The earlier the condition is found, the quicker treatment can begin.
