Strategies For Treating Pericarditis
Pericarditis is an inflammation of the pericardium, a membrane that protects the heart. It can be either acute or chronic, and it may be caused by a car accident or other chest trauma. Pericarditis can also develop due to inflammatory conditions such as lupus and rheumatoid arthritis, and it may occur as a result of cancer, tuberculosis, or kidney failure. Symptoms of this condition typically include left-sided chest pain that gets worse when breathing in, heart palpitations, a low-grade fever, shortness of breath while lying down, and a cough. Patients may also experience swelling of the abdomen or lower limbs, and they may feel a general sense of weakness or fatigue.
To check for pericarditis, a clinician will first listen to the chest with a stethoscope. They will check for the presence of a pericardial rub, an abnormal sound indicative of this illness. The pericardial rub is created when the pericardial layers rub together. To confirm a diagnosis of this condition, electrocardiograms, echocardiograms, chest x-rays, and CT scans may be needed.
Pericardiectomy

A pericardiectomy is a surgical procedure that removes some or all of the pericardium. This operation is normally recommended for patients who have developed constrictive pericarditis, a complication of acute or chronic pericarditis. Constrictive pericarditis causes the pericardium to become rigid and scarred, reducing the heart's ability to function and potentially resulting in heart failure. The pericardiectomy procedure is performed under general anesthesia, and it requires making an incision in the sternum.
After cutting the sternum, the surgeon will be able to reach the heart and remove the pericardium. They will then wire the sternum and ribs back together, and the wound will be closed with stitches. Patients usually stay in the hospital for up to seven days after the surgery, and recovery time at home is approximately six to eight weeks. While recovering at home, patients should avoid lifting items. Patients normally see their cardiologist for a follow-up appointment and echocardiogram six weeks after the operation.
Avoid Strenuous Activity

Rest is one of the most effective treatments for pericarditis, particularly acute pericarditis. In fact, mild cases of this condition may resolve with rest and the use of over-the-counter pain relievers. Doctors recommend that patients with any form of pericarditis avoid strenuous activity, which can be a trigger for chest pain and other symptoms of the condition.
In particular, patients should avoid lifting heavy items and participating in intense exercise sessions. While light activity may be safe, it is important for patients to ask their cardiologists for individualized advice about appropriate levels of activity during their treatment. Keeping a symptom diary, in which patients record their symptoms and anything they were doing when the symptoms started, can help clinicians plan the most appropriate care for the patient.
Pain Relief Medication

Pain relief medication is necessary in nearly all cases of pericarditis. For mild cases, ibuprofen and other over-the-counter anti-inflammatory medications may be effective. Most doctors recommend patients take six to eight hundred milligrams of ibuprofen up to three times a day. The ibuprofen should be taken in this way for two weeks, and patients may then discontinue it if their pain has resolved. For moderate to severe pain, prescription pain relievers, including narcotic medications, may be needed. Cardiologists often advise patients to take colchicine with ibuprofen.
Colchicine is an anti-inflammatory that can reduce the duration of pericarditis, and it may also lower a patient's risk of developing a future episode of the condition. Patients with kidney disease or liver problems should not take colchicine, and they may be prescribed an alternate medication. While taking pain relievers, patients should always report any new pain to their physicians, and they may wish to keep a symptom diary to share at their medical appointments.
Pericardiocentesis
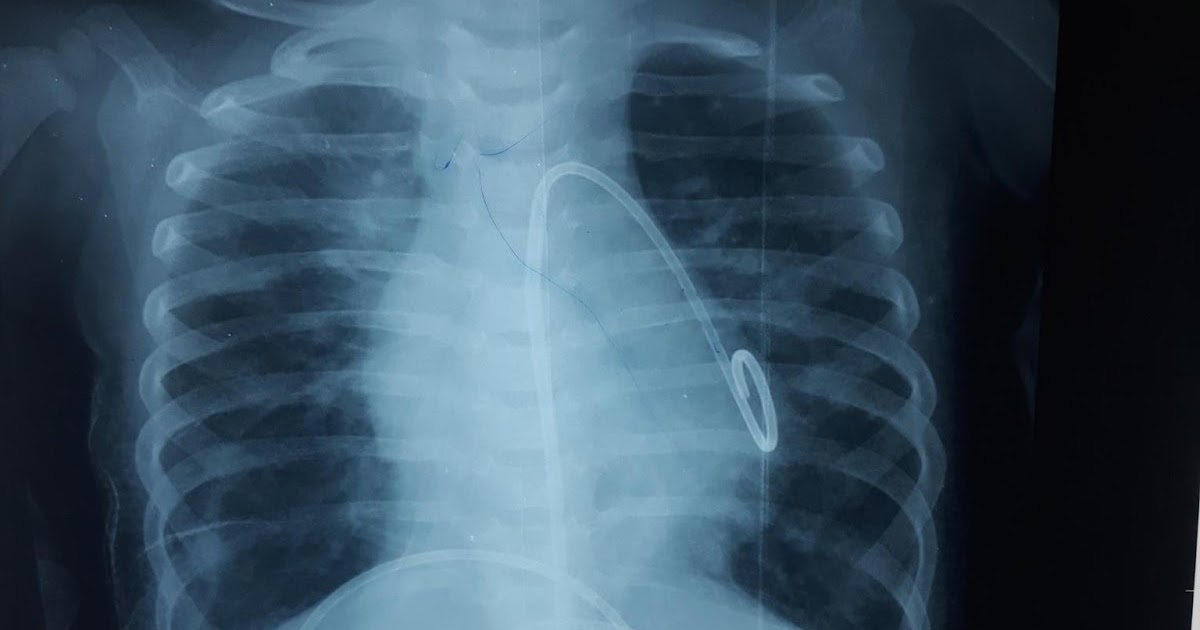
Pericardiocentesis is an emergency intervention used to treat cardiac tamponade, one of the possible complications of pericarditis. Cardiac tamponade develops when an excessive amount of fluid accumulates within the pericardium, and a pericardiocentesis drains the excess fluid. Doctors may use ultrasounds and echocardiograms to monitor the heart during the procedure. After numbing the skin near the breastbone with a local anesthetic, the doctor will insert a needle into the pericardium.
While inserting the needle, the clinician will use live imaging to ensure the needle reaches the correct location. Next, the needle will be withdrawn and replaced with a catheter, which will be attached to a bag outside the body, and fluid from the pericardium will drain into the bag. The drainage may continue for several days, and patients will be closely monitored during this time. Occasionally, it may not be possible for the doctor to drain enough fluid from the pericardium with this technique. If this happens, a pericardial window may be performed instead. This involves making a small incision in the pericardium, and the fluid drains into the chest cavity.
Corticosteroids

Corticosteroids are medications that reduce inflammation throughout the body, and they can also reduce pain. These medications are used in pericarditis patients who have severe chest pain that does not respond to over-the-counter pain relievers and colchicine. Prednisone is one of the most commonly prescribed corticosteroids for patients with pericarditis.
While taking this medication, patients should be aware of potential side effects, which include unusual weight gain, an irregular heartbeat, blurry vision, vomit that looks like coffee grounds, and swelling in the hands or feet. Some patients may also feel weak and develop muscle cramps, and signs of infection, including fevers and sore throats, have been reported. Patients should report these and any other new or worrying side effects to their healthcare team as soon as possible.
