Watch Out For These Early Warning Signs Of Glaucoma
Glaucoma is a term used to describe a group of progressive eye disorders that eventually lead to blindness. The two most common types of glaucoma are primary open-angle glaucoma and angle-closure glaucoma. Open-angle glaucoma begins by working inward and eventually leads to tunnel vision. Acute angle-closure glaucoma tends to cause blurred vision with halo effects around the eyes. Both cause irreversible damage, though this damage is at least somewhat treatable provided glaucoma is detected in the early stages of the condition. In order to detect glaucoma early, it is vital to be aware of the different and early warning signs of the condition. Knowledge is key here!
Sudden Vision Changes

It may seem like a no-brainer, but any sudden changes to an individual’s vision is a good enough reason for them to get checked out by an eye doctor. Sudden vision changes in one or both eyes may be a sign of severe problems such as retinal damage. Any sudden visual disturbance in dim lighting is an early sign of acute angle-closure glaucoma. Individuals should talk to their primary doctor or optometrist if they notice any other changes in their vision, such as trouble seeing far away objects. Even if the issue is not glaucoma, it is still crucial for early identification so the appropriate actions can be taken.
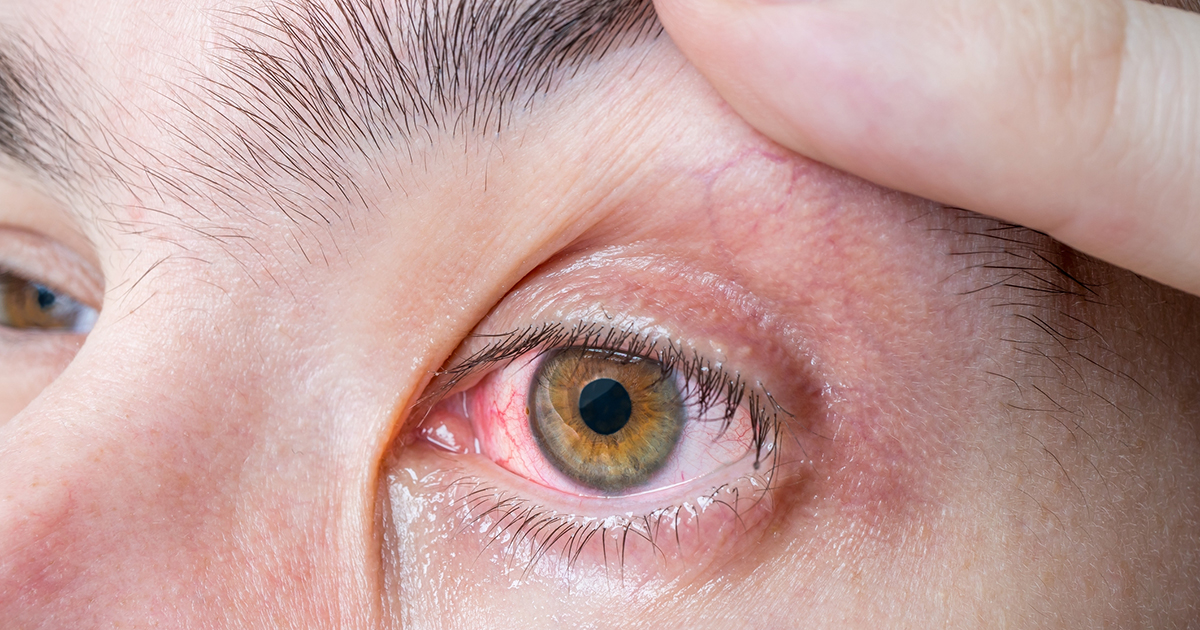
Redness And Swelling

Bloodshot or swollen eyes may be an indication of pressure buildup within the eye, which is a sign of acute angle-closure glaucoma. Eye pressure occurs when the iris becomes inflamed and causes the sensation of pressure within the eye. By the time the eyes become visibly swollen and red, emergency treatment or surgery might be necessary, depending on the circumstances and what exactly is causing it. Patients may also experience redness in their eyes if they overuse eye drops, are dehydrated, or are overtired.
Nausea

Nausea is most commonly linked to digestive upset, but it can also be the result of impaired vision. If an individual’s vomiting and nausea occur along with severe eye pain, it could be an indication of acute angle-closure glaucoma. Eye pain may present itself in the form of a headache, which can be confused with the flu, particularly when accompanied by digestive ailments like nausea. If the pain and nausea last for more than two weeks, it could be an indication of vision problems.
Tunnel Vision

Tunnel vision can quite literally look like the individual is seeing through a tunnel. It typically occurs during late-stage primary open-angle glaucoma and develops as a gradual narrowing of the person’s peripheral vision. Tunnel vision interrupts the individual’s ability to see the edges or corners of whatever they are looking at directly. Unfortunately, many individuals do not realize their sight is becoming limited or narrowing until later stages of the disease. If individuals notice any changes in their peripheral vision, even small ones, they should see an eye doctor immediately.
Blurry Vision

Blurry vision is a common indication of poor eyesight. But if an individual notices their vision is becoming progressive blurry, it might be a sign of acute angle-closure glaucoma. Visual acuity occurs when there is a gradual decline in the sharpness of your vision. Because it does not usually present itself until later stages of the disease, it is important for affected individuals to seek treatment as soon as they notice blurry vision as significant damage may be irreversible, even with surgery.
Halos
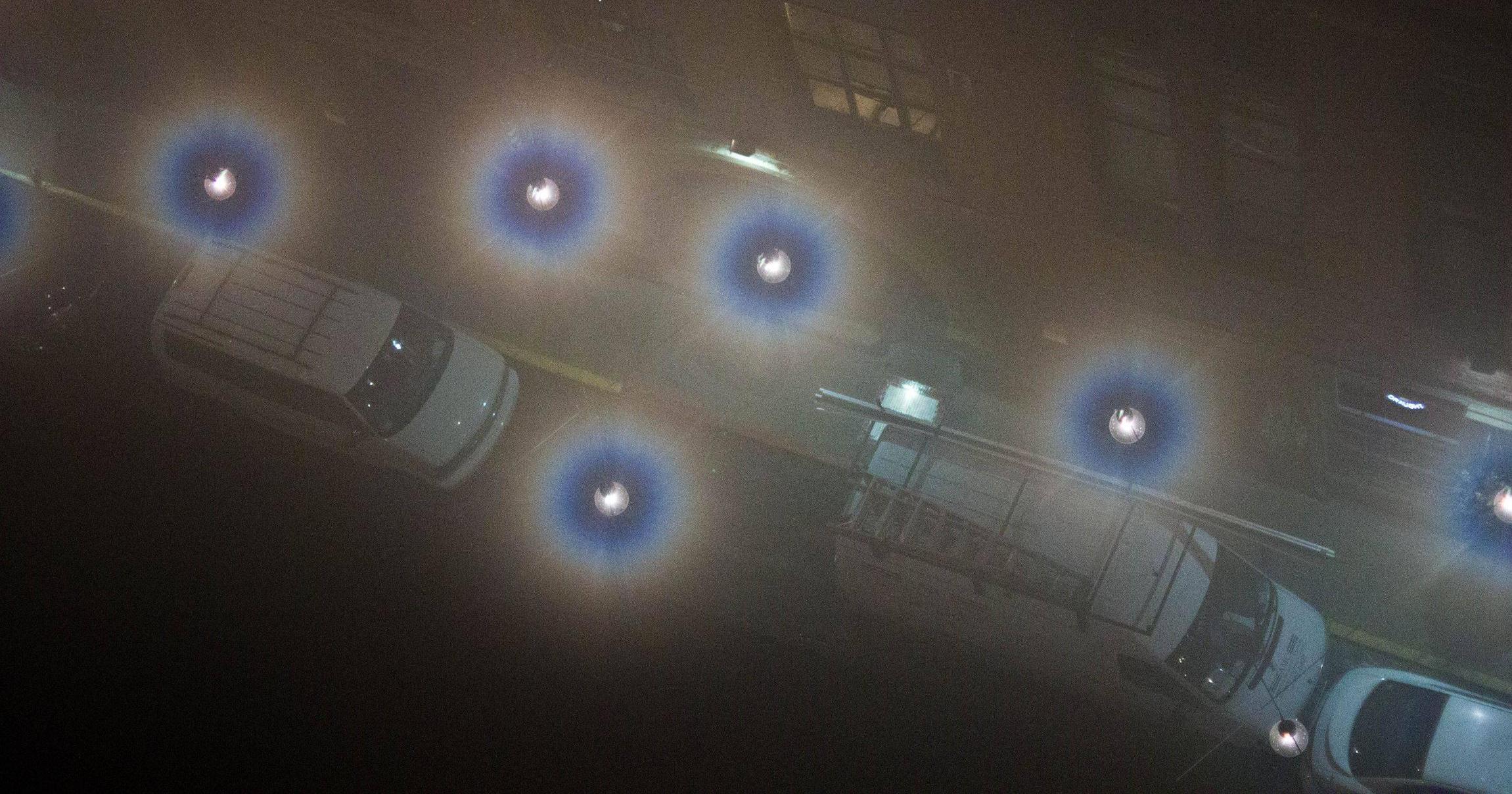
Most individuals tend to notice something is not right with their eyes when they start having trouble seeing at night. This can make driving very difficult and even dangerous. Acute angle-closure glaucoma may cause halos, or a rainbow effect when light shines in an individual’s eyes at night. This can cause lights to seem blurry. Halos are sometimes accompanied by extreme pressure at night while trying to drive. If an individual’s vision becomes blurry at night or in other dim light areas, they should talk to a doctor about treatment.
Visible Changes To The Eye

Glaucoma is not usually detectable by the naked eye, but if individuals notice a gradual shift in the appearance of their eyes, it might be an early sign. Patients with acute angle-closure glaucoma may develop a reddish tint in their eyeballs. They may also have large pupils that do not dilate in the light. The cornea, or the transparent covering of the eye, may also appear cloudy or swollen. Those who notice any of these changes in themselves or someone they know should seek treatment right away.
Eye Pain

Pain is usually always the number one indicator something is wrong in the body. If an individual experiences sudden eye pain or headaches behind their eyes, it may be a sign of late-stage acute angle-closure glaucoma. Those who notice an onset of pain suddenly in or around their eyes should seek treatment immediately to prevent vision loss or even blindness in the years to come. If glaucoma is detected, the doctor may schedule surgery or take other preventative actions. Even if the source of the pain is not related to glaucoma, it is better to see an optometrist for an eye check-up and ensure there are no other underlying conditions.
Patchy Blind Spots
An individual who begins to experience the appearance of patchy blind spots may be affected by glaucoma. These patchy blind spots typically occur when an individual's glaucoma has progressed to the degree of causing their optic nerve to incur damage. The optic nerve is the component of the eye responsible for the transmission of visual information to the vision centers in the brain. The optic nerve contains over a million tiny nerve fibers that originate from the retina. The fluid an individual's eye produces (aqueous humor) is meant to drain from the eye through a net-like structure, and it then flows into the individual's blood stream. Most individuals affected by glaucoma have a problem with this system of aqueous humor drainage from the eye. The aqueous humor is unable to drain and begins to accumulate in the eye, compressing the small fibers of the optic nerve and other components of the eye. Over time, this malfunction leads to permanent damage as the optic nerve fibers begin to die off. This mechanism is what causes a glaucoma patient to see patchy blind spots in their peripheral vision.
Mid-Dilated Pupil

A mid-dilated pupil in an individual's eye can indicate they are suffering from angle-closure glaucoma. This type of glaucoma occurs when the eye cannot drain aqueous humor due to a specific mechanism. The iris in the eye is the part that contains color. The pupil is the black structure in the center of the iris. The lens of the eye sits right behind the pupil and iris and is held in place by ligaments. The ciliary body is the muscular structure that sits behind the iris that produces aqueous humor, which flows into the cornea and pupil and is then drained through the net-like structure at the junction where the iris and cornea meet. The mid-dilated pupil happens during a sudden occurrence of angle-closure because most contact between the lens and the iris happens when an individual's pupil is in a mid-dilated position. The net-like structure where the aqueous humor should drain from becomes obstructed, and the pressure in the eye increases. This increasing pressure causes a restriction of blood supply to the muscle that controls the dilation of the pupil. The muscle becomes non-functional as a result, and the pupil remains in the mid-dilated position. This mechanism is why a mid-dilated pupil can indicate acute angle closure glaucoma.
High Intraocular Pressure
An individual may exhibit high intraocular pressure as a manifestation of their glaucoma. Intraocular pressure is a measurement that can indicate how much pressure is inside of the eye. Intraocular pressure is measured in millimeters of mercury (mmHg). A healthy intraocular pressure is in between ten and twenty-two mmHg, while high intraocular pressure is characterized by a measurement of over twenty-two mmHg. Elevated intraocular pressure is present in the majority of individuals affected by glaucoma, but it is not a symptom that appears in all affected individuals. This high pressure does not cause the patient to feel pain, but it will result in other symptoms when the optic nerve becomes damaged. High intraocular pressure may occur due to a mechanism that causes the eye to produce more aqueous humor than it should, or because of a dysfunction in the process of aqueous humor drainage from the eye. With an overproduction of aqueous humor, the net-like structure meant to drain the fluid is unable to keep up with the production of it. This malfunction causes it to accumulate, and pressure levels increase within the eye. When a mechanism is disabling the aqueous humor drainage system, the fluid backs up in the eye and raises intraocular pressure. Both situations commonly occur in individuals with glaucoma.
