10 Essential Facts About Opioids: What They Are & How They Affect You
In a world grappling with chronic pain, opioids emerge as a double-edged sword: a powerful balm capable of profound relief, yet fraught with significant risks. Derived from the ancient poppy plant or crafted in a lab, these potent substances interact with your brain's pain receptors, fundamentally altering how you perceive discomfort. While a short course of medication like morphine can offer crucial respite from severe pain, their seductive power quickly escalates the danger of dependence and addiction. Understanding opioids isn't just about their pain-killing prowess; it's about grasping their intricate nature and profound impact. Delve into 10 essential facts to truly comprehend what opioids are, how they work, and why their influence extends far beyond mere pain relief.
1. How Do Opioids Work?
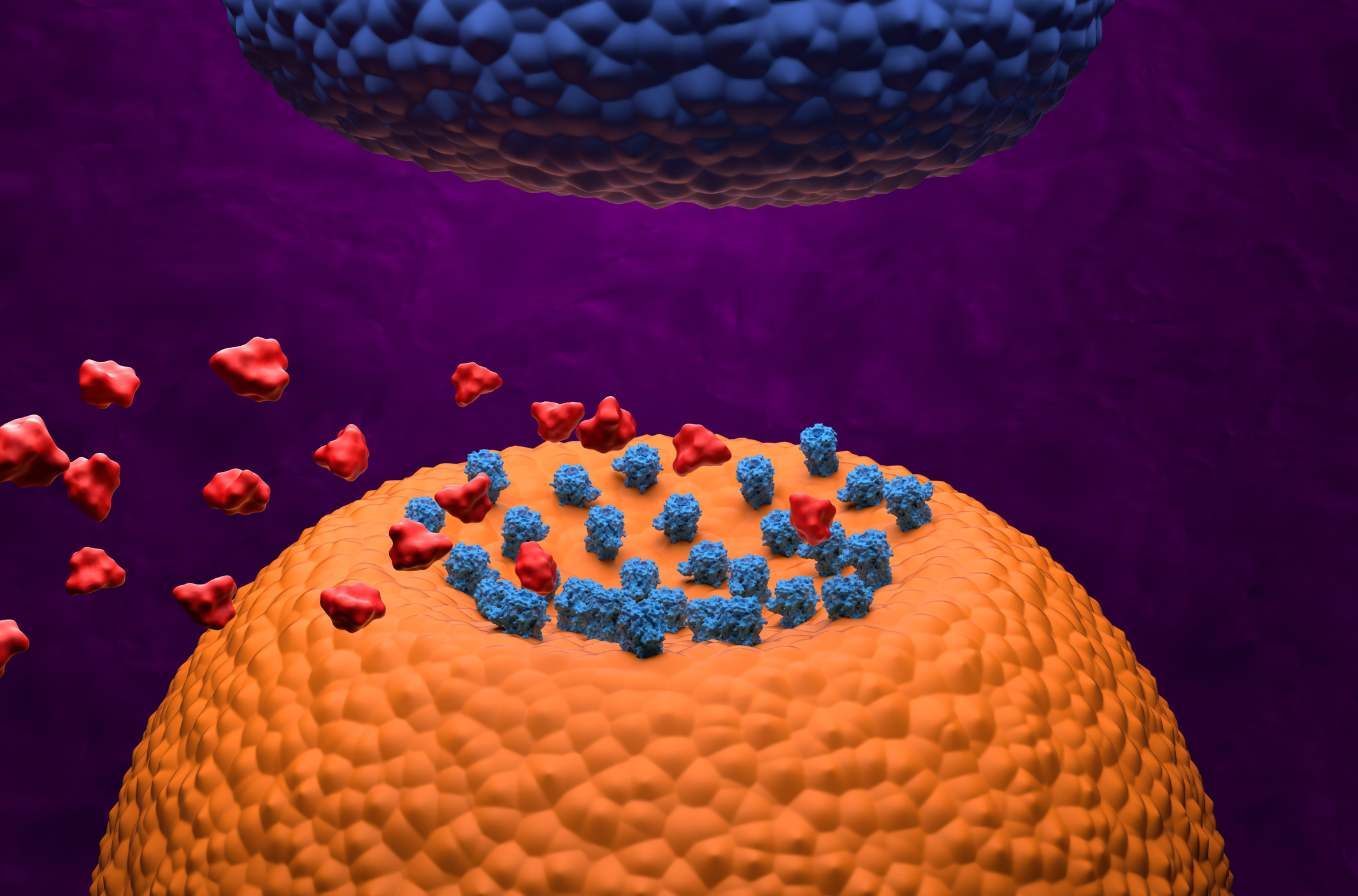
Once an opioid molecule is present in the bloodstream, it travels to the brain, where it attaches itself to specific receptors. These receptors are also found in the spinal cord and other areas of the body. It is then able to mimic neurotransmitters based on its structure, activating certain cells. Think of an opioid and its targeted receptor as a lock and key, as it initiates a chemical response in the brain's reward center. Working differently than a natural neurotransmitter, opioids do not activate nerve cells in the same manner. As opioids take effect, the reward center is flooded with dopamine, supporting movement, emotion, cognition, motivation, and pleasure. It is the stimulation of this circuit that places individuals at-risk for drug abuse and a potential dependence. Based on its rewarding properties, individuals must follow all instructions carefully and continually review their dosage with a physician. Next, discover what opioids exactly do to the human body.
2. How Are Opioids Used?

Commonly prescribed for pain, opioids can be used in a wide range of clinical settings. After a patient is out of surgery, for instance, opioids may be given to help control pain levels. The same is true for those who have experienced a significant injury, are enduring cancer-related pain, or require relief from a chronic, degenerative disorder. The human body actually produces its own opiate-like substances, such as endorphins. Unfortunately, our body’s natural defense system is not effective against immense levels of pain. Considering pain is the body’s way of letting a person know that something is abnormal, powerful opioids are generally used to combat pain levels. Keep reading to learn about the short-term effects of opioids.
3. Short-Term Effects

There are various short-term effects that opioids can have on an individual’s body, and can affect both their physical and mental well-being. Some of the short-term physical effects of opioid use include drowsiness, constipation, nausea and vomiting, and difficulty breathing, which can also worsen sleep apnea. Male patients may also experience impotence due to using this medication, even for a short period of time. Mental effects of opioid use include experiencing feelings of euphoria or feeling high, as well as headaches, dizziness, and confusion, which can cause an individual to lose their balance and fall, resulting in possible fractures or other injuries. Continue reading to find out what the long-term effects of opioid use can do to the body.
4. Long-Term Effects

The long-term effects of using opioids can also include an increased tolerance to it, substance use disorder or dependence, liver damage, infertility in women, worsening pain also known as opioid-induced hyperalgesia, and life-threatening withdrawal symptoms in infants born to addicted mothers. Even when opioids are prescribed by a physician for pain management and relief, some of the serious side effects include a physical dependence, substance use disorder, and the possibility for the patient to overdose. Individuals who end up dealing with an opioid dependence problem are likely to experience intense withdrawal symptoms when they lower their dosage quickly or suddenly stop using the medication. If a patient wants to lower their dosage, they should do so with the help of a healthcare provider. Next, discover the various types of opioids that are used for pain relief.
5. Opioids For Pain Relief

When taken as prescribed, an individual will experience temporary pain relief and reduced anxiety. When administered in higher doses, intense feelings of euphoria are reported. They are also prescribed in cases relating to irritable bowel syndrome (IBS) and chronic obstructive pulmonary disease (COPD). If a person is experiencing chronic pain, it is suggested that they try other options before resorting to opioids, as a long-term use is not recommended, and that they also consult a physician when it comes to taking opioids for pain relief. Some of the most common opioids are codeine, fentanyl, hydrocodone, methadone, and oxycodone. Often prescribed on an ‘as needed’ basis, it is important to regularly check in with a doctor if someone is taking these potent medications. If an individual has been taking opioids for an extended period of time, they should speak with their doctor before fully discontinuing use, as they may experience symptoms of withdrawal.
6. The Insidious Nature of Tolerance and Physical Dependence

Beyond simple addiction, understanding tolerance and physical dependence is crucial. Tolerance means your body adapts, requiring higher doses to achieve the same pain relief. Physical dependence occurs when your body needs the opioid to function "normally," leading to withdrawal symptoms if stopped suddenly. This isn't addiction (which involves compulsive drug-seeking), but it's a dangerous precursor. A doctor might prescribe a taper to gradually reduce dosage, managing dependence and preventing severe withdrawal, which can be unexpectedly debilitating.
7. Opioid-Induced Hyperalgesia: When Pain Gets Worse

One of the most paradoxical and concerning long-term effects is opioid-induced hyperalgesia (OIH). Instead of continuous pain relief, the opioid actually increases your sensitivity to pain, making non-painful stimuli hurt, and existing pain feel even more intense. This phenomenon is a serious risk of prolonged use, where the very medicine intended to relieve suffering ironically amplifies it. Recognizing OIH is vital, as it often necessitates a change in pain management strategy rather than increasing the opioid dose.
8. The Respiratory Depression Risk: A Silent Threat

Opioids primarily reduce pain, but their most dangerous side effect is respiratory depression – slowing or stopping breathing. This is the main cause of fatal overdoses. Opioids suppress the brain's signals to breathe, making it a critical concern, especially when combined with other central nervous system depressants like alcohol or benzodiazepines. Even prescribed doses can lead to this if there are underlying conditions or drug interactions. Understanding this fundamental risk underscores the need for strict dosage adherence and emergency preparedness (like Narcan).
9. The Brain's "Rewiring": Beyond the Reward Center

Opioid use fundamentally rewires neural pathways beyond just the pleasure/reward center. Chronic exposure can alter the brain's stress response system, decision-making circuits, and impulse control mechanisms. This isn't merely about feeling good; it's about deep, structural changes that contribute to compulsive drug-seeking behaviors and make quitting incredibly challenging. Understanding this neurobiological impact reveals why addiction is a complex brain disease, not just a failure of willpower.
10. Naloxone (Narcan): The Life-Saving Antidote

Despite the risks, a critical life-saving tool exists: naloxone (brand name Narcan). This medication rapidly reverses opioid overdose by blocking opioid receptors in the brain, restoring normal breathing within minutes. It's safe, non-addictive, and now increasingly available without a prescription. Knowing about naloxone, how to administer it, and keeping it on hand if someone you know is at risk of opioid overdose, can be the difference between life and death. It's an essential part of the opioid safety conversation.
Navigating the Opioid Landscape: Knowledge is Your Safest Path

Opioids represent a complex medical frontier, offering powerful relief while harboring significant dangers. From their intricate dance with your brain's receptors to the silent threats of respiratory depression and hyperalgesia, understanding these 10 essential facts is paramount. This isn't just medical jargon; it's vital information empowering you to engage safely with their use. Whether you or a loved one relies on them, remember: informed decisions, strict adherence to medical guidance, and awareness of emergency measures like naloxone are your strongest defenses. Knowledge transforms vulnerability into vigilance, ensuring responsible pain management and safeguarding lives.
