7 Common OTC Painkillers That Could Be Hurting Your Gut Microbiome
Our gut is home to a thriving community of trillions—yes, trillions—of bacteria that help digest food, keep immunity strong, and support everything from mood to metabolism. This intricate “microbiome” is as unique as our fingerprint, quietly working behind the scenes day after day. But have you ever wondered how everyday medications might be affecting this delicate system? Over-the-counter painkillers seem like harmless fixes for aching backs or headaches, often considered staples in medicine cabinets. Yet, a wave of new research shines a light on how some of these familiar pills could be shifting the balance in our guts in ways we’re only beginning to understand. It turns out even the medicines we rely on most for quick pain relief may have far-reaching effects beyond their original target. If you use painkillers regularly, you’re not alone—these medications are incredibly common. The good news? Knowing more empowers us to make choices with confidence and care. Here’s an evidence-based look at seven of the most commonly used painkillers, what the science says about their gut effects, and gentle steps you can take to look after both comfort and microbiome health.
1. Ibuprofen (Advil, Motrin): The Everyday Pain Reliever with Unexpected Gut Risks

Among the lineup of over-the-counter painkillers, ibuprofen is the all-star—almost everyone reaches for it at some point. Known for targeting pain and inflammation, it’s found in products like Advil and Motrin. But recent studies are starting to change how we think about its effects on the gut. In 2025, University of South Australia researchers concluded that ibuprofen can lead to notable shifts in gut bacteria, encouraging mutations that may even help bacteria resist antibiotics. While these microscopic changes might not be noticeable overnight, they have sparked concern among scientists, especially for people who take ibuprofen routinely for headaches, joint pain, or muscle aches. Ibuprofen’s primary job is to dial down inflammation, but in the process, it can also disturb the balance of helpful and potentially harmful gut microbes. If you find yourself relying on ibuprofen often, it’s a great time to chat with your healthcare provider about options, or consider practices that may protect your gut, like taking the lowest effective dose and not combining with other similar meds unless advised. Remember, moderation is key—and your gut will thank you in the long run.
2. Acetaminophen (Tylenol): A Surprising Contributor to Microbial Shifts

Acetaminophen, known as Tylenol, may feel like the “gentle” option for sensitive stomachs. For years, it’s been recommended as a safe go-to for headaches, fevers, or minor aches. But new research is giving experts pause. In an eye-opening 2025 study, acetaminophen turned out to have a surprising downside—it increased mutation rates in gut bacteria when used alongside certain antibiotics, potentially driving resistance. This happens because acetaminophen seems to help bacteria activate their own microscopic “defense shields,” making them harder to combat if infections arise. While this doesn’t mean you need to stop using Tylenol for the occasional ache, if it’s your pain reliever of choice several times a week, it’s worth discussing with your doctor. The emerging science reminds us that what feels soothing up top can have ripple effects for the trillions of organisms we rely on every day. Mindful use and regular check-ins with your care team can keep both pain and your inner ecosystem in harmony.
3. Diclofenac (Voltaren): Potent Relief, Potential Microbiome Stirring

Diclofenac is a heavy hitter in the pain-relief world, especially for arthritis, muscle soreness, and sports injuries. Marketed as Voltaren and available in both oral and topical forms, it can offer targeted relief when stiffness refuses to budge. But this potency has a flip side—research shows diclofenac may disrupt the gut’s protective lining and alter how bacteria thrive. Its ability to reduce inflammation can also disturb the balance of the gut microbiome, especially if used regularly or at higher doses. While most commonly prescribed, some OTC products are readily available in pharmacies and online, making it easy to overdo. Older adults and those managing chronic pain may be especially at risk. When reaching for diclofenac, consider alternating with non-drug strategies (like physical therapy or gentle activity), and don’t hesitate to ask your healthcare professional for personalized advice. Small tweaks in your approach may go a long way toward keeping both your joints and your gut supported.
4. Aspirin: Classic Painkiller under the Gut Health Microscope

Aspirin may be the original over-the-counter pain medication—the one your grandparents trusted for everything from headaches to heart health. While millions still rely on its low-dose form to help prevent cardiovascular problems, research on how aspirin impacts gut bacteria is only just getting started. Some studies and expert opinion suggest that, like other NSAIDs, aspirin may tip the gut’s microbial balance, possibly allowing less-desirable bacteria to flourish. Solid proof is still emerging, and the full implications are not yet clear. Still, if you routinely take aspirin or use combination medications containing it, it pays to be mindful. If your plan includes low-dose aspirin for heart wellness, talk to your doctor before making any changes. As always, the best strategy is using only what’s needed—while keeping an eye on your gut’s “silent partners” in health.
5. Naproxen (Aleve): Prolonged Action, Possible Microbial Disruption

Naproxen, commonly found under the brand name Aleve, is another staple for easing long-lasting aches—think arthritis, back pain, or menstrual cramps. Its ability to tame pain for hours makes it a favorite for those who need sustained comfort. However, prolonged or frequent use may have consequences for the gut. Like other NSAIDs, naproxen can irritate the stomach lining and, new evidence suggests, alter the mix of bacteria in the gut. While much of the research is grouped with ibuprofen’s effects, early findings point to a similar risk for disturbing the microbiome. If Aleve is part of your regular routine, try to take “gut breaks” when you can, stick to the recommended dose, and incorporate gut-friendly foods or habits. A simple log of when and how you take these medications can also provide helpful patterns for you and your doctor to review together.
6. Tramadol: Prescription-Strength Relief Now OTC in Some Regions
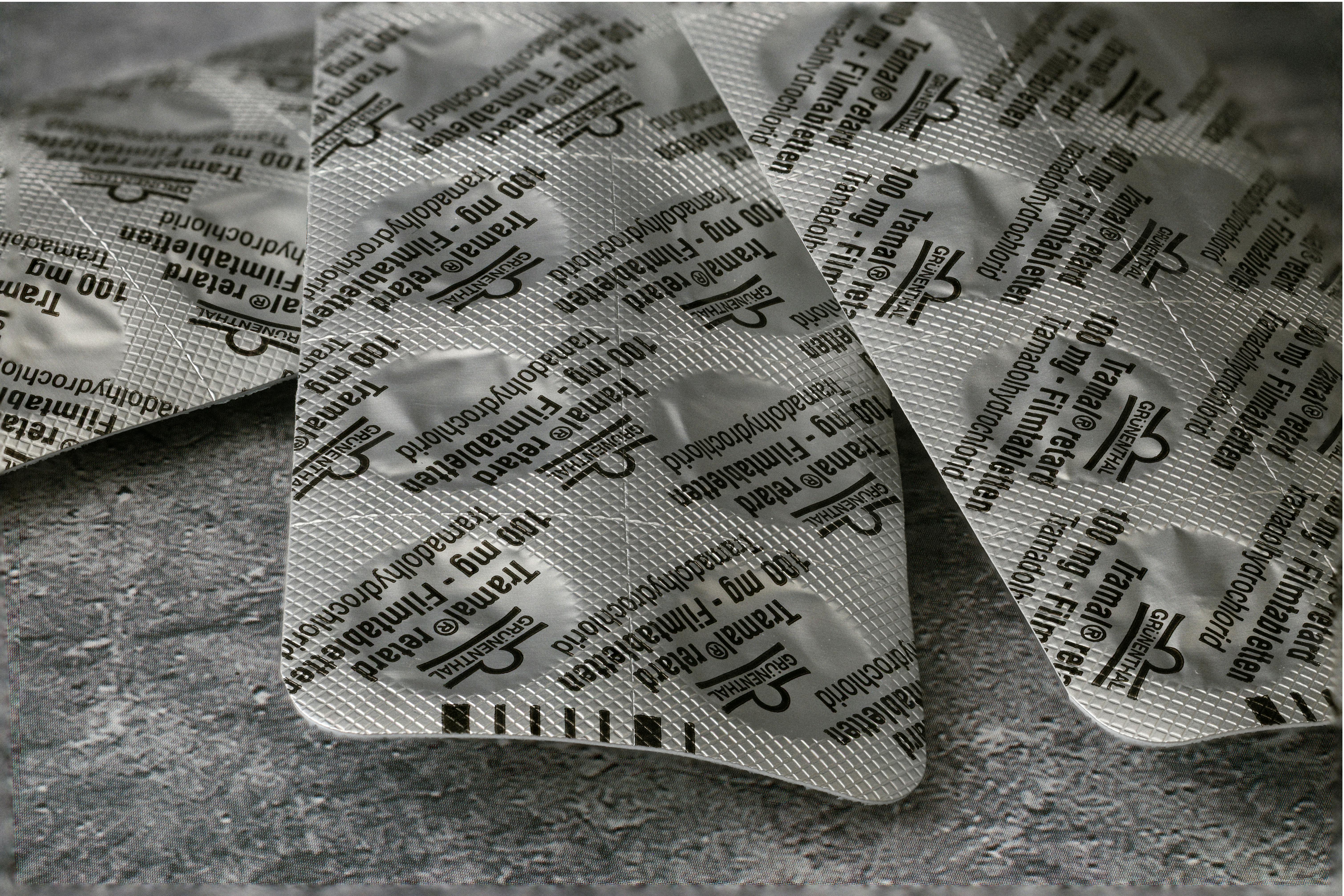
Tramadol belongs to a different class than most OTC painkillers, but is sometimes available without a prescription in limited formulations. Frequently given for more serious or chronic pain, especially after injuries or surgeries, tramadol was highlighted in recent microbiome research for its role in driving bacterial mutation and resistance. The gut seems to respond to tramadol by changing both the number and types of bacteria present, which may make antibiotics less effective down the line. While tramadol remains prescription-only in the US for most uses, it’s important to recognize its presence in combination products or in other countries’ OTC aisles. If you have been prescribed tramadol, consider reviewing your entire medication list with your provider—especially if you’re taking several painkillers routinely. Gut health is just one reason among many to approach all medicines with self-compassion and steady support.
7. Combination Painkillers: Double-Edged Swords for Gut Health

Walk through the pharmacy and you’ll spot countless products that blend two or more pain-relieving ingredients. Whether it’s aspirin plus acetaminophen, or ibuprofen paired with caffeine, these combinations can promise fast, powerful relief. But research is starting to reveal a catch: mixing painkillers may multiply their effects on the gut microbiome—potentially fueling more robust changes, resistance, or microbial imbalance than a single agent alone. This is especially important for those who juggle chronic pain and take several medications daily, including prescription drugs. Before doubling up, check medications for overlapping ingredients, and be candid with your health team about everything you use (including non-prescription supplements). By coordinating your approach, you protect more than comfort—you honor the many ways your gut and daily wellness are connected.
Gentle Steps to Support Both Comfort and Gut Health
While pain is an inevitable part of life, how we manage it can have deep-reaching effects on our bodies, including the trillions of helpful microbes that call our gut home. Occasional use of over-the-counter painkillers is safe for most people, but paying attention to frequency, dosage, and combinations can help preserve both comfort and gut balance. If you take pain medications often—or find your list of daily pills growing—consider starting a simple log to track what you use and how you feel, and always bring these notes to conversations with your healthcare team. There’s no one-size-fits-all answer, but informed choices go a long way. Small tweaks, gentle curiosity about side effects, and a willingness to ask questions can make all the difference on your wellness path. Most importantly, don’t halt or switch medications abruptly without guidance. Your gut microbiome is a powerful partner in health, adapting as you do. By honoring both symptom relief and hidden helpers inside, you’ll be moving toward vibrant, sustainable wellness—one kind decision at a time.
