Guide To Colon Cancer Causes And Risk Factors
Colon cancer is a malignancy that originates in an individual's large intestine or colon. Colon cancer can develop in an individual of any age but is more common in older adults. Symptoms of colon cancer include changes in stool consistency, frequent diarrhea, frequent constipation, blood in the stool, cramping, abdominal discomfort, excessive gas, the sensation of incomplete bowel emptying, weight loss, fatigue, and weakness. Most individuals who do not have numerous risk factors begin getting screened for colon cancer when they reach the fifth decade of life.
Colon cancer is diagnosed with the use of blood tests, CT scans, and a procedure called a colonoscopy. Should the physician discover any areas that look suspicious during a colonoscopy, they can biopsy the suspicious tissue during the procedure. Treatment for colon cancer includes surgery to remove the malignancy if possible, chemotherapy, and radiation therapy.
Family History Of Colon Cancer

Individuals who have a family history of colon cancer are more likely to develop this type of malignancy in their colon. Malignancy anywhere in the body is caused by a change or mutation in cellular DNA that causes the cells to grow rapidly, multiply excessively, and live longer then they should. Some of the mutations that cause cancer can be inherited from an individual's parents. While this cause of colon cancer is relatively uncommon, specific inherited syndromes like familial adenomatous polyposis and hereditary nonpolyposis colorectal cancer can significantly increase an individual's risk of developing colon cancer.
A patient's chance of developing colon cancer is even higher when they have more than one blood family member who has been affected by colon or rectal cancer at some point in their life. Between five and ten percent of all cases of colon cancer are the result of an inherited genetic factor or syndrome. An individual who has a family history of polyp development in the colon or a condition that causes them is also at an increased risk of developing colon cancer.
History Of Colon Polyps
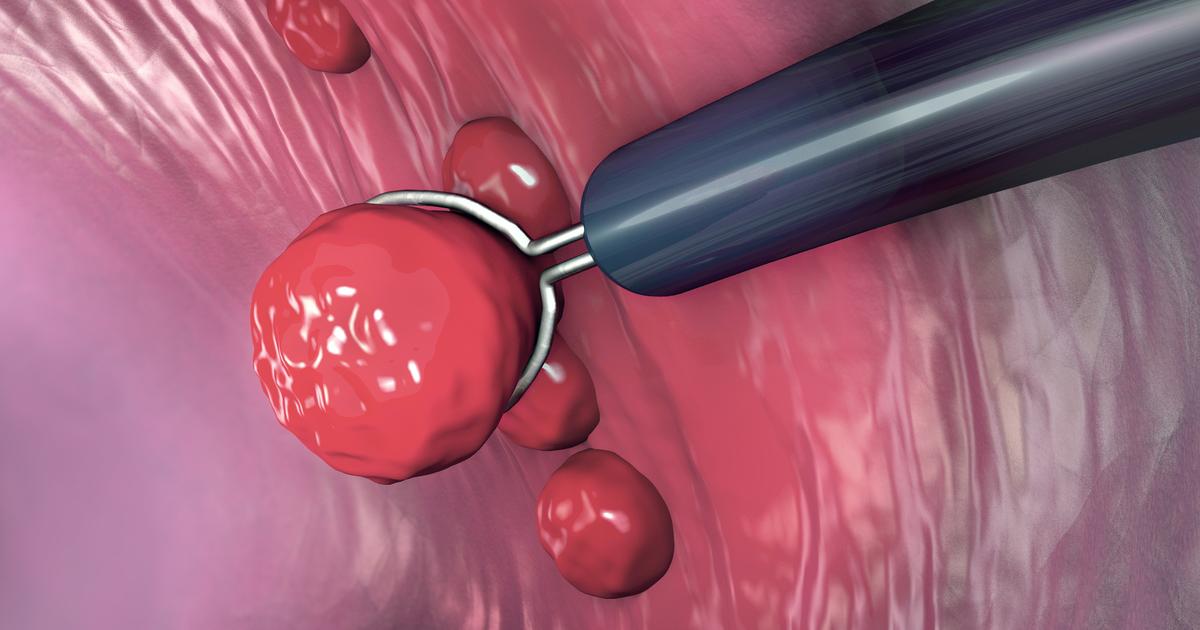
An individual who has a history of colon polyps is at a higher risk of developing colon cancer than an individual who does not. A colon polyp is an abnormal tissue growth that occurs inside of the colon or large intestine. Polyps come in different shapes and sizes. The most common kind of polyp known to increase an individual's risk of developing colon cancer is called an adenomatous polyp. These types of polyps are often associated with mutations in the DNA of cells that make up the large intestine lining.
This malfunction means the larger an adenomatous polyp grows, the more likely it is to incur a DNA mutation that causes the development of colon cancer. Colon polyps can only be found with a procedure referred to as a colonoscopy. Most adenomatous polyps do not produce any symptoms, so most individuals are unaware they have them until they undergo a routine colonoscopy. Colon polyps are removed as soon as they are found to prevent the development of colon cancer.
