Complications Linked To Muscular Dystrophy
Muscular dystrophy is the overarching term for a group of diseases that lead the body to become progressively weaker and lose muscle mass. The condition is caused by abnormal gene mutations that interfere with the body's ability to produce proteins that help form healthy muscles. Because there are multiple types of muscular dystrophy, the complications and age of onset vary. The symptoms also vary depending on what muscle groups are affected.
The most common variety begins showing symptoms in childhood, but other types don't cause symptoms until an individual reaches adulthood. While muscular dystrophy doesn't have a cure, there are medications and physical therapy options that can help slow the disease and manage overall symptoms.
Heart Problems
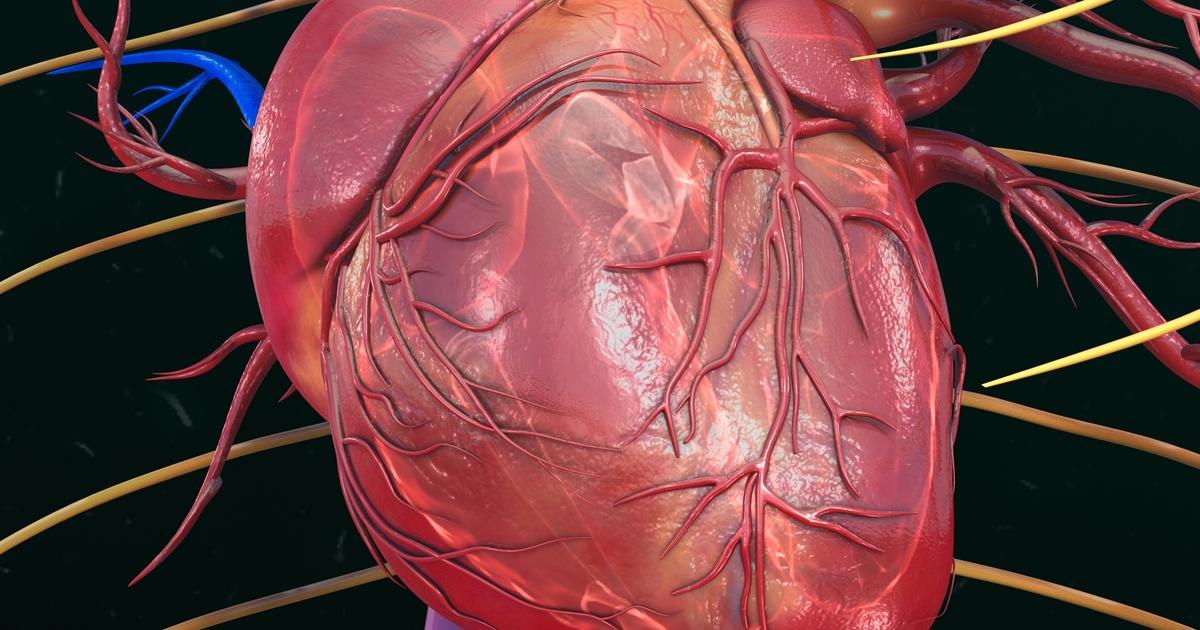
Research has shown multiple types of muscular dystrophy include cardiac dysfunction. Depending on the case and the underlying subtype, some people might experience heart problems as the main symptom of the illness. Because muscular dystrophy tends to be a rare issue, and each subtype is also rare, cardiologists might struggle to provide a diagnosis for the heart issues. Until recently, researchers weren't aware of how often cardiomyopathy causes death in muscular dystrophy patients. However, recent advances in respiratory care have improved survival rates. It's important to detect muscular dystrophy-related heart problems early.
While it might not be possible to stop the heart issues from developing, instituting heart-healthy therapies can sometimes help to slow the progression of the disease. Echocardiography and electrocardiography tests are recommended for screening patients for heart disease. There has also been some research indicating cardiovascular magnetic resonance screening can reveal early heart involvement in muscular dystrophy patients. The most common types of this condition including the heart are those that affect dystrophin proteins, like Becker and Duchenne muscular dystrophy. Other types that show involvement are Emery-Dreifuss, limb-girdle, and myotonic.
Trouble Walking

Muscular dystrophy can cause trouble walking, though the amount of leg involvement varies depending on the type. Some patients might progress to the full use of a wheelchair, while others may only need mobility devices like braces. The condition can also cause difficulty standing up. Duchenne muscular dystrophy is the most commonly recognized subtype, and it tends to show symptoms in childhood. Patients with this form usually have such progressive muscle weakness they need to use a wheelchair before they reach their teens.
Because of how rapidly the disease progresses and how it impairs the heart and lungs, children with this disease don't usually live past their twenties. Becker muscular dystrophy has similar symptoms to Duchenne, but it also occurs between eleven and twenty-five years old, and the severity is less pronounced. Patients with Becker muscular dystrophy might walk on their toes, fall frequently, experience muscle cramps and spasms, and struggle to get up from the floor.
