10 Milky Mysteries Unveiled: The Sneaky Suspects Behind Lactose Intolerance
Ever felt a surprising gurgle, bloating, or discomfort after enjoying what should be a simple meal? You're not alone. What if that seemingly innocent dairy treat is secretly sabotaging your comfort? Lactose intolerance, a digestive mystery affecting an astonishing 75% of the global population, often lurks behind these frustrating symptoms. It’s more than just a sensitivity to milk; it’s a complex inability to break down lactose, the sugar found in dairy. But the culprits aren't always obvious. Beyond the expected glass of milk, hidden sources and unexpected triggers can be silently turning your system upside down. Join us as we unveil 10 milky mysteries – the sneaky suspects behind lactose intolerance – empowering you to identify the true cause of your discomfort and reclaim your digestive peace.
1. Insufficient Production Of Lactase

The primary cause of lactose intolerance is insufficient production of lactase, an enzyme produced in the small intestines. This enzyme is responsible for the digestion of lactose, and patients who have low levels of the enzyme will experience symptoms of lactose intolerance after consuming dairy. In patients with lactase deficiencies, foods that contain lactose move into the colon instead of being digested properly before reaching this area. The presence of lactose in the colon triggers symptoms. If patients with lactose intolerance do not want to completely eliminate dairy products, there are several types of dairy milk available made without lactose, and patients could also try taking a lactase enzyme supplement prior to consuming dairy. The supplements reduce symptoms for many patients.
2. Increasing Age

Increasing age is a major risk factor for lactose intolerance. The condition is most often diagnosed during adulthood, and it is much less common in infants and children. The body's production of lactase naturally declines with age, and this can eventually lead to the symptoms of lactose intolerance. Since these symptoms could be caused by a number of other conditions that are potentially serious, older adults who believe they may be lactose intolerant should consider visiting a gastroenterologist for a full evaluation. The specialist can perform a detailed abdominal exam and other tests to check for irritable bowel syndrome, Crohn's disease, and other related conditions. If an older patient is diagnosed as lactose intolerant, they may wish to consult a nutritionist for help in creating a meal plan that includes sufficient calcium and vitamin D intake. In particular, older adults may need to take dietary supplements to meet their nutritional needs, especially if they already have other underlying health conditions.
3. Bacterial Overgrowth In The Small Intestine
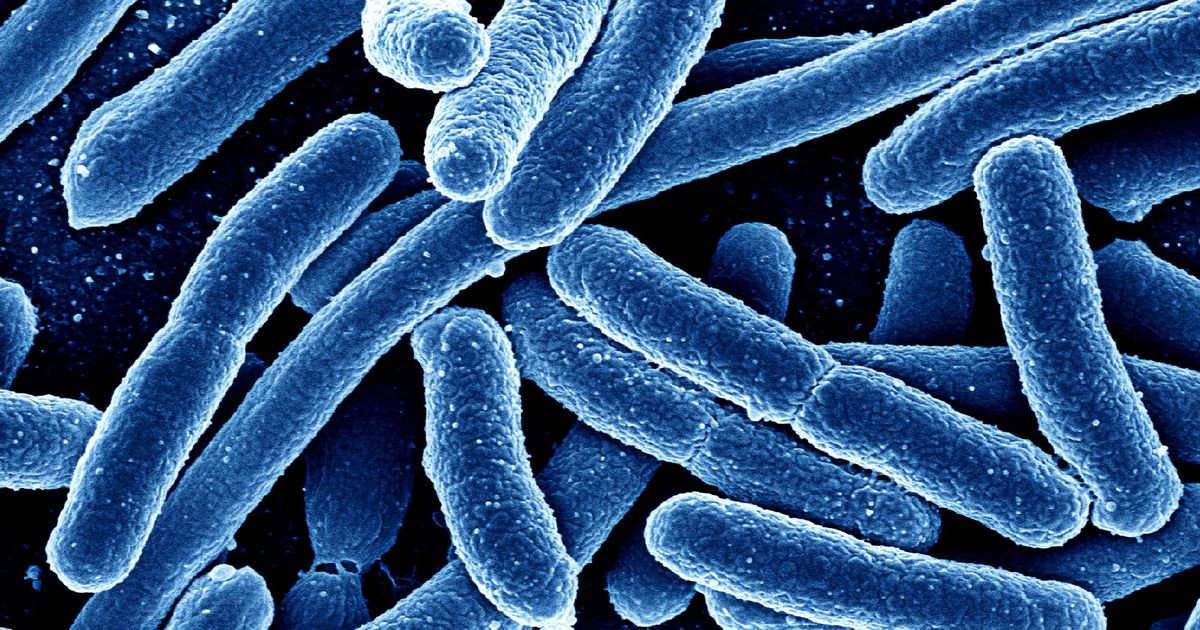
Bacterial overgrowth in the small intestine is a recognized medical condition related to lactose intolerance, and it triggers many of the same symptoms. In addition to the symptoms of lactose intolerance, patients with an excessive amount of abnormal bacteria in the small intestine might experience fatigue and constipation, and nausea is common. Individuals with severe forms of the disease could lose weight unintentionally, and iron deficiency anemia may develop. Patients who have weakened immune systems, including individuals with lupus, and those who have had abdominal surgery are at an increased risk of this kind of bacterial overgrowth. To check for the condition, doctors use a lactulose breath test. Similar to the hydrogen breath test, the lactulose test involves the patient drinking a lactulose solution and breathing into a balloon at fifteen-minute intervals for a three-hour period. The breath samples are considered positive for bacterial overgrowth if either hydrogen or methane is present. To treat bacterial overgrowth, doctors generally use antimicrobial herbs and antibiotics such as rifaximin and neomycin. Patients are asked to follow a low-FODMAP diet.
4. Ethnicity

Ethnicity is a strong risk factor for the development of lactose intolerance. The condition is more prevalent among Hispanics, American Indians, and patients of African or Asian descent. These patient populations may have a genetic form of lactose intolerance caused by a mutation in a gene that manufactures lactase. Known as hypolactasia, this disease begins during childhood, and it is especially common among individuals of Asian descent. Parents who have hypolactasia may wish to consider having their child tested for the condition. If it is present, patients may need to work with a gastroenterologist and a nutritionist to manage symptoms and ensure adequate nutrition, particularly for infants and children. While individuals with some forms of lactose intolerance can still tolerate small amounts of dairy, individuals with hypolactasia may prefer to consume a dairy-free diet to control their symptoms as effectively as possible. Patients with this condition should always report any new or worsening symptoms to their healthcare team, and they may need to attend periodic follow-up appointments.
5. Certain Cancer Treatments

Individuals undergoing certain cancer treatments can develop lactose intolerance as a side effect. For these patients, lactose intolerance may present after active treatment has finished too. In particular, radiation therapy to the abdominal area is associated with a strong risk of developing lactose intolerance, and it might develop due to intestinal complications following chemotherapy. Patients being treated for cancer should ask their oncology team about their individual risk of developing lactose intolerance as a side effect of their treatment, and they may wish to consult with a nutritionist about starting a lactose-free or lactose-reduced diet during their cancer treatment to minimize any painful symptoms. If necessary, doctors can prescribe medications for these patients to reduce nausea and diarrhea.
6. Crohn's Disease and Other Inflammatory Bowel Diseases (IBD)

Beyond just bacterial overgrowth, inflammatory bowel diseases like Crohn's disease or ulcerative colitis can be sneaky culprits. These chronic conditions cause inflammation and damage to the lining of the digestive tract, including the small intestine where lactase is produced. This direct damage can significantly impair the body's ability to produce sufficient lactase, leading to secondary lactose intolerance. For individuals with IBD, managing their underlying disease is critical, but a temporary or long-term lactose-free diet might also be necessary to alleviate persistent digestive discomfort.
7. Celiac Disease (Undiagnosed or Poorly Managed)

Celiac disease, an autoimmune condition where gluten consumption damages the small intestine lining, is another surprising link to lactose intolerance. The constant inflammation and damage to the intestinal villi (finger-like projections responsible for nutrient absorption and enzyme production) directly impair lactase production. For many undiagnosed celiac patients, lactose intolerance symptoms may be one of their first noticeable digestive issues. Adhering to a strict gluten-free diet is essential for healing the intestine, which can, in turn, restore lactase production and alleviate lactose intolerance in many cases.
8. Gastric Bypass Surgery and Other Abdominal Surgeries

Major abdominal surgeries, particularly gastric bypass procedures, can surprisingly trigger or worsen lactose intolerance. These surgeries alter the normal digestive pathway, sometimes bypassing sections of the small intestine where lactase is produced or where lactose is typically digested. This can lead to rapid transit of food to the colon, causing undigested lactose to ferment. Patients undergoing such procedures should be aware of this potential side effect and discuss dietary adjustments with their medical team to manage symptoms effectively post-surgery.
9. Acute Gastroenteritis (Post-Infectious Lactose Intolerance)

A severe bout of acute gastroenteritis, often caused by viral (e.g., rotavirus) or bacterial infections, can surprisingly lead to temporary lactose intolerance. The inflammation and damage to the small intestine lining from the infection can temporarily reduce lactase enzyme production. This "post-infectious lactose intolerance" is usually transient, with lactase levels typically recovering as the intestinal lining heals over weeks or months. However, awareness is key, as reintroducing dairy too soon can prolong discomfort and recovery.
10. Certain Parasitic Infections

While less common in many Western countries, certain parasitic infections of the gut, such as giardiasis or cryptosporidiosis, can also be sneaky causes of temporary lactose intolerance. These parasites directly damage the small intestine lining, interfering with its ability to produce lactase. If you experience persistent digestive issues including lactose intolerance-like symptoms after traveling to areas where these parasites are common, or after exposure to contaminated water, seeking a diagnosis and treatment for the underlying infection is crucial to resolve the intolerance.
Your Digestive Peace: Unveiling the Milky Mysteries

The discomfort of lactose intolerance often extends beyond the obvious glass of milk, woven into a complex tapestry of causes that affect a vast majority of the global population. We’ve unraveled 10 surprising truths, from the genetic predispositions of ethnicity and the natural decline with age, to unexpected culprits like past infections, certain surgeries, and even common autoimmune conditions. Armed with this knowledge, you are empowered to pinpoint the true source of your symptoms. Understanding these "milky mysteries" isn't just about dietary avoidance; it's about making informed choices to reclaim your digestive comfort and truly nourish your body.
