15 Mind-Bending Mazes in The Landscape of Mental Health Conditions
Mental health isn’t a single diagnosis or a one-size-fits-all experience—it’s a vast, intricate landscape made up of diverse conditions that affect how people think, feel, and function. While awareness has grown, misunderstanding and stigma still cloud the conversation. Too often, mental illness is reduced to caricatures, missing the complexity—and humanity—of those who live with it. Each condition is its own maze: winding, unpredictable, and deeply personal. And every individual’s journey through it is unique. That’s why we’ve expanded our guide to 15 Mind-Bending Mazes in the Landscape of Mental Health Conditions—to help unravel the nuance, foster empathy, and encourage proactive care. Whether you’re seeking clarity for yourself or insight into someone else’s experience, understanding the architecture of these conditions is a powerful first step.
1. Mood Disorders

Mood disorders are mental health conditions that cause serious emotional disruption. Ordinarily, an individual's moods and emotions change in response to external stimulation. For example, individuals might feel irritable and tired if they're under a lot of stress. At the same time, patients should experience positive feelings in response to things like happy social interaction, hobbies, and meeting goals. Certain factors can influence mood in a neurotypical individual like nutrition, sleep, and hydration. When someone has a mood disorder, though, their emotions don't match the circumstances surrounding them. The best-known mood disorder is major depression. A depressed individual doesn't experience the same pleasure in their life as a neurotypical person does, even if they try to inject positive things. Another mood disorder is bipolar disorder, which combines depression and mania. Mania can include feelings of euphoria, agitation, paranoia, panic, and reduced impulse control. With bipolar disorder, the changes in mood come seemingly out of nowhere rather than having external triggers. Seasonal affective disorder is a type of depression that occurs in the winter months, and persistent depressive disorder is a low-grade, chronic kind of depression.
2. Anxiety Disorders

Occasional stress and anxiety are normal parts of life. When individuals are re feeling pressure or worried about the future, it's natural to respond with anxiety. But an anxiety disorder elevates this to another level. Anxiety disorders occur when a person has persistent, excessive, intense fears and worries regarding day-to-day life. There are many different kinds of anxiety disorders, some of which only show symptoms in specific circumstances. An anxiety disorder causes panic and fear that interferes with daily functioning. Affected individuals might avoid certain situations and experiences out of fear, and they might also have trouble enjoying life because they're so consumed by stress and panic. Several anxiety disorders manifest with panic attacks. These are brief periods of intense fear that cause similar sensations to a heart attack, but they don't tend to last longer than ten minutes. Generalized anxiety disorder involves a generally heightened sense of anxiety and catastrophe about all aspects of life. Social anxiety disorders are related to fear of social situations. Debilitating phobias are classified as anxiety disorders. Obsessive-compulsive disorder is also an anxiety disorder that causes panic when an individual doesn't follow through on their compulsions.
3. Psychotic Disorders

Psychotic disorders are mental health issues that affect a patient's cognition and perception of the world. Different disorders present with different symptoms. Though many villains in mainstream media experience psychosis, actual psychotic individuals are much more likely to be victims of violent crime than perpetrators. In fact, psychotic individuals do not have a rate of violent action any higher than the general population. An individual with a psychotic disorder may struggle to think rationally and make judgments based on logic. They may believe things that aren't true and have inappropriate emotional responses to things. Communication can sometimes be difficult as well. Psychotic disorders can cause severe symptoms that make day-to-day function difficult. However, the majority of these illnesses can be treated through a combination of medication and therapy. Schizophrenia is one of the best-known and most misunderstood psychotic disorders. It includes hallucinations and delusions, along with internal symptoms like distorted thought patterns. Schizoaffective disorder combines schizophrenia symptoms with a mood disorder.
4. Eating Disorders

Eating disorders are mental health conditions that present with disturbances in an individual's eating behaviors, thoughts about eating, and emotions about eating. The hallmark symptoms of eating disorders involve a preoccupation with food and body weight. At any given moment, millions of individuals are dealing with eating disorders. They are most prevalent in women between twelve and thirty-five years old, but anyone can develop an eating disorder. The three main eating disorders are bulimia nervosa, anorexia nervosa, and binge eating disorder. Anorexia and bulimia often present with an obsessive sense of perfectionism, feelings of low self-worth, and self-criticism. Patients with anorexia and bulimia may create elaborate rules and rituals regarding food to establish a sense of control over their lives. It's common for anorexic and bulimic individuals to have intense fears about weight gain and being fat, which are often combined with poor self-image. Binge eating disorder involves periods of overeating without purging. It's the most common eating disorder in the United States. The binges are often used to self-medicate feelings of low self-worth or unhappiness.
5. Personality Disorders

Personality disorders are slightly different from other types of mental health issues. They tend to be more difficult to treat, though medication can sometimes be helpful depending on the case. With personality disorders, counseling and therapy are a much more integral part of treatment than medication. An individual's personality is the set of characteristics that set them apart from others, and it includes behaviors, feelings, and thoughts. Personality disorders are patterns of behavior, emotion, and thought that last for long periods, cause mental distress or issues with functioning, and deviate from cultural expectations. There are ten types of personality disorder currently outlined in the DSM-V. A personality disorder must affect at least two of these: a person's way of viewing themselves and others, their emotional responses, their relationships with others, and their ability to control their behavior.
6. Obsessive-Compulsive and Related Disorders

OCD is more than being tidy or liking things symmetrical—it’s about intrusive thoughts and compulsive actions that disrupt daily life. Obsessions are distressing, persistent thoughts, while compulsions are repetitive behaviors meant to reduce anxiety. These rituals don’t bring relief for long and often escalate over time. Related disorders include body dysmorphic disorder (preoccupation with perceived flaws), hoarding disorder, and trichotillomania (hair-pulling). These conditions aren’t quirks—they’re serious and often misunderstood. Effective treatment combines cognitive behavioral therapy, particularly exposure and response prevention, and sometimes medication. Understanding that these behaviors are rooted in anxiety—not choice—can shift how we view those affected.
7. Trauma and Stressor-Related Disorders
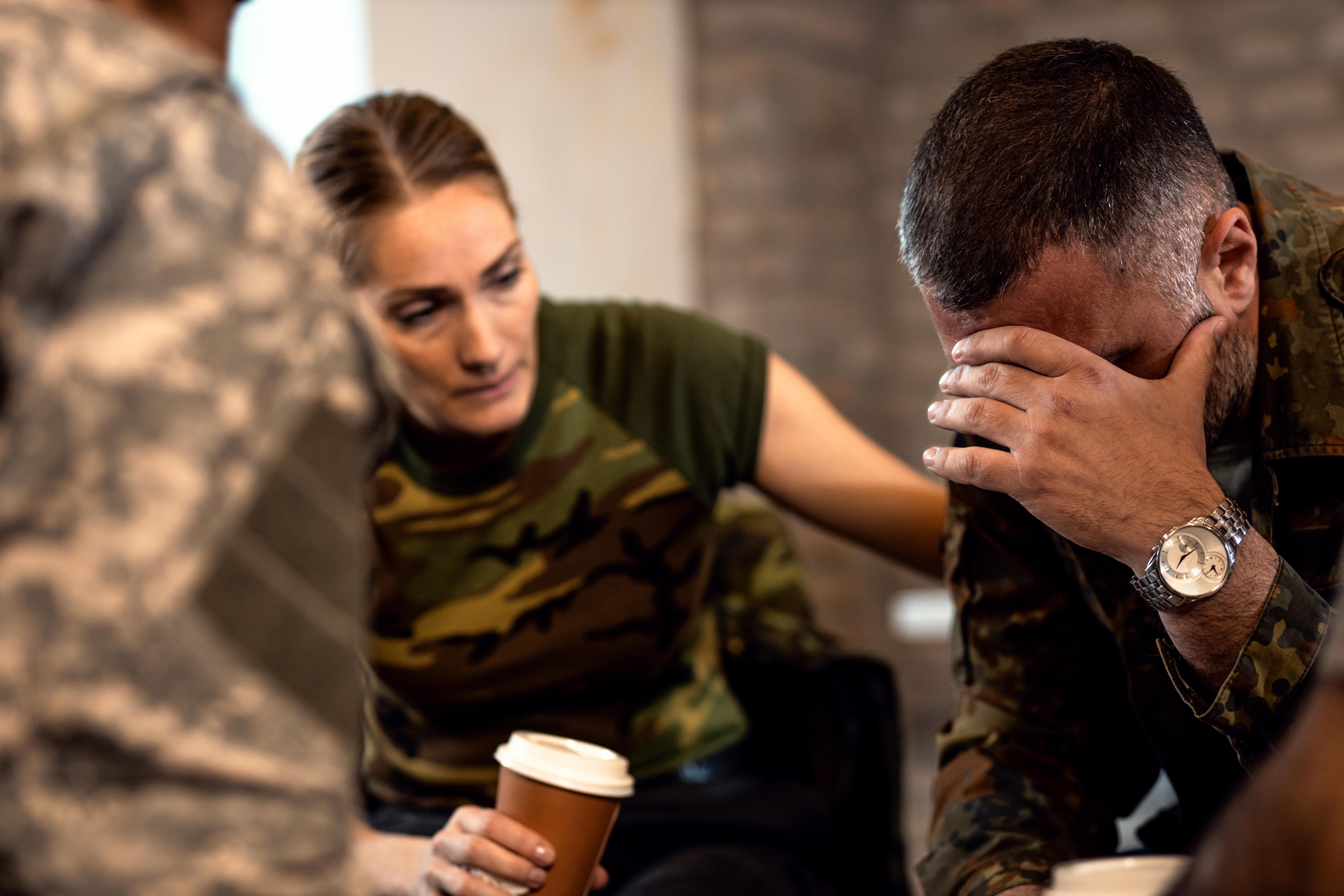
Not everyone who goes through trauma develops a disorder—but for some, the aftermath rewires everything. Trauma and stressor-related disorders arise after deeply distressing experiences, including abuse, war, loss, or accidents. Post-traumatic stress disorder (PTSD) is the most well-known, involving flashbacks, hypervigilance, and emotional numbness. There’s also acute stress disorder (short-term PTSD), and adjustment disorder, which surfaces after a major life change. Children may develop reactive attachment disorder from early neglect. These aren’t just about the past—they shape how a person sees safety, trust, and self-worth. Trauma-informed care is essential, focusing on empowerment, stability, and building new emotional pathways.
8. Neurodevelopmental Disorders
Neurodevelopmental disorders begin in childhood but often persist into adulthood. They affect how the brain grows and functions, influencing behavior, learning, and communication. Autism spectrum disorder (ASD) ranges widely in presentation—from nonverbal individuals to those with high intellectual ability but social struggles. ADHD impacts attention, impulsivity, and executive function. Other examples include specific learning disorders like dyslexia and intellectual disabilities. These aren’t deficiencies—they’re differences. Early support, accommodations, and inclusive understanding can transform lives. With the right tools, many individuals with neurodevelopmental disorders thrive academically, socially, and professionally. Labels help identify needs—but they never define worth.
9. Dissociative Disorders

Dissociative disorders are often a psychological escape route when the mind is overwhelmed. They involve disruptions in identity, memory, or sense of self. Dissociative identity disorder (formerly multiple personality disorder) features two or more distinct identities that control behavior at different times. Dissociative amnesia may cause someone to forget key life events, especially after trauma. Depersonalization-derealization disorder leads to feeling detached from one’s body or surroundings, as if in a dream. These are protective mechanisms gone awry—not attention-seeking or dramatic behavior. Therapy aims to integrate fractured parts of the self, rebuild trust, and create emotional safety.
10. Somatic Symptom and Related Disorders

In these disorders, emotional distress surfaces as physical symptoms. Somatic symptom disorder causes excessive focus on pain, fatigue, or other health concerns—even when no clear medical cause exists. Illness anxiety disorder (formerly hypochondriasis) involves an intense fear of having or developing a serious illness. Conversion disorder manifests emotional trauma as neurological symptoms—paralysis, tremors, or seizures with no medical basis. These aren’t “all in your head”—they’re real, lived experiences of suffering. The mind and body are deeply connected, and untreated psychological distress can manifest physically. Treatment blends medical support with psychotherapy to address the emotional roots.
11. Impulse-Control and Conduct Disorders

These disorders involve difficulty resisting harmful impulses—toward self, others, or property. Intermittent explosive disorder includes episodes of sudden, intense aggression that feel uncontrollable. Conduct disorder, often diagnosed in youth, includes violating rules, lying, theft, or cruelty. Oppositional defiant disorder features persistent defiance, anger, and argumentativeness, especially toward authority. These aren’t simply “bad behavior” or poor parenting—they often stem from trauma, inconsistent environments, or neurodevelopmental challenges. Early intervention, therapy, and consistent boundaries can make a dramatic difference. Compassion matters—especially when patterns of harm are really patterns of pain.
12. Sleep-Wake Disorders

Sleep isn’t just rest—it’s regulation. Sleep-wake disorders disrupt the body’s internal clock, affecting mood, memory, and physical health. Insomnia disorder involves chronic difficulty falling or staying asleep, while hypersomnolence leads to excessive sleepiness during the day. Narcolepsy causes sudden sleep attacks and can be socially and professionally disruptive. Circadian rhythm disorders misalign sleep schedules with social expectations. Untreated sleep issues are linked with anxiety, depression, and cognitive decline. But sleep therapy, good sleep hygiene, and in some cases, medication, can dramatically restore quality of life. Mental health and sleep are cyclical—when one suffers, the other often follows.
13. Sexual and Gender Identity Disorders (Now Classified Under Gender Dysphoria)

It’s crucial to approach gender and sexuality in mental health with care and clarity. Gender dysphoria is not about identity itself—but the significant distress caused when one’s gender identity doesn't align with their assigned sex. This condition is deeply misunderstood and often politicized, but it’s rooted in real psychological pain. Treatment is individualized and may include therapy, social transition support, and medical care such as hormone therapy or surgery. Validation, not erasure, is key. Gender dysphoria is no longer viewed as a disorder of identity, but of distress—and support can lead to empowered, authentic lives.
14. Substance-Related and Addictive Disorders

Addiction is not moral failure—it’s a complex mental health issue involving brain chemistry, behavior, and often trauma. These disorders include dependence on alcohol, opioids, stimulants, or other substances that affect the mind. They also encompass non-substance addictions like gambling disorder. Substance use becomes a coping mechanism that rewires reward circuits, leading to compulsive behavior despite harmful consequences. Recovery isn’t linear—and it rarely happens in isolation. Treatment involves detox, counseling, social support, and sometimes medication-assisted therapy. Compassion, structure, and harm reduction go further than punishment ever will. Healing is possible—with help.
15. Paraphilic Disorders

Paraphilic disorders involve intense, persistent sexual interests that deviate from normative patterns—and cause distress or harm. Not all atypical sexual interests are disorders; what defines a paraphilic disorder is when the behavior involves non-consenting individuals or causes significant psychological distress. Examples include voyeuristic disorder, exhibitionistic disorder, and pedophilic disorder. These are sensitive and often criminally relevant topics, requiring clinical expertise, legal attention, and strict ethical care. But treating paraphilic disorders also matters for public safety, prevention, and psychological rehabilitation. It's a controversial area—but mental health must engage with the hard topics too, not just the sympathetic ones.
Mental health isn’t just about diagnoses—it’s about stories, survival, and the silent battles people fight every day. These 15 mind-bending mazes show that mental health conditions aren’t linear or predictable; they’re complex terrains that shape how individuals move through the world. No two paths are alike, even when names or symptoms overlap. Some people live in loops of anxiety, others in the fog of dissociation or the chaos of mood swings. But in every case, understanding unlocks compassion. Treatment opens doors. And talking about it—honestly, openly—chips away at stigma. If you or someone you know is struggling, know this: the maze might be confusing, but you don’t have to navigate it alone. Support, therapy, and recovery aren’t just possible—they’re powerful. The more we educate ourselves and each other, the more we build a world where mental health isn’t whispered about—it’s respected, prioritized, and met with care.
