Surprising Twists and Turns of a Bone Marrow Biopsy Journey
The words "bone marrow biopsy" can sound daunting, conjuring images of discomfort and uncertainty. Yet, this vital procedure—where a tiny sample from inside your bone is carefully examined—offers an unparalleled window into your body's most essential factory: your bone marrow. It’s where your blood cells are born, and when something’s amiss, a biopsy provides crucial answers that other tests simply can't. Far from being a mysterious ordeal, understanding this outpatient procedure and its 21 surprising twists and turns can transform apprehension into assurance. Join us as we demystify this critical diagnostic journey, from the initial steps to what those results truly mean for your health.
1. What Is Bone Marrow?
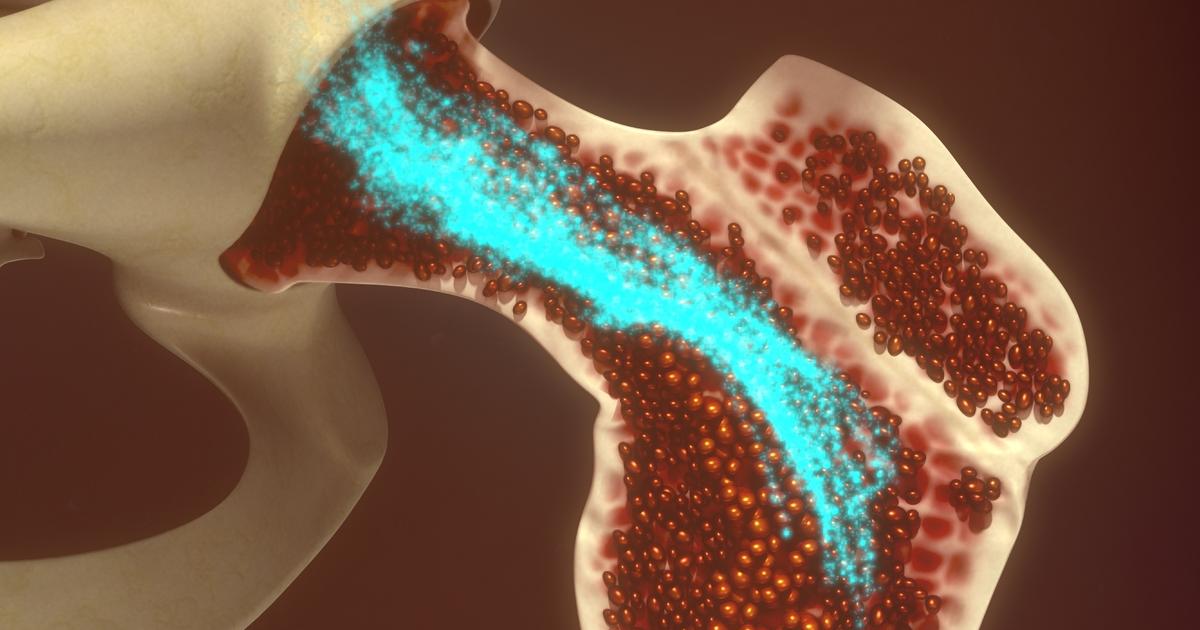
Bone marrow has two different physical components: a liquid portion and a solid portion. A bone marrow aspiration procedure is utilized to remove the liquid physical component of the bone marrow for analysis, where a bone marrow biopsy is utilized to extract and examine the solid physical component of the bone marrow. In the center of the bones, there is a hollow area referred to as the medullary cavity. Inside the medullary cavity are the soft tissues that make up bone marrow. Bone marrow contains red bone marrow or myeloid tissue and yellow bone marrow or fatty tissue. The bone marrow in a healthy individual produces over 200 billion new blood cells each day. The red bone marrow does most of the work in the production of new blood cells, but yellow marrow can revert to red marrow in circumstances that warrant it, like fever or blood loss. Bone marrow produces white blood cells of different variations that can survive anywhere from a few hours to several days. It also produces red blood cells that last for 120 days and platelets that last for ten days.
2. When A Biopsy Is Needed

A bone marrow biopsy may be ordered by a physician if patients have abnormal levels of red blood cells, white blood cells, or platelets. An individual who has unexplained anemia may need to undergo a bone marrow biopsy to identify its cause. A bone marrow biopsy can identify diseases of the bone marrow, including myelodysplastic syndrome or myelofibrosis, and conditions that affect the blood cells, such as leukopenia, polycythemia, and thrombocytopenia. A bone marrow biopsy can aid in the diagnosis of certain types of cancer that affect bone marrow and blood components, such as leukemias and lymphomas. A bone marrow biopsy can determine if a patient has a genetic disorder called hemochromatosis, where iron inappropriately accumulates in the blood. A bone marrow biopsy can help identify the cause of a patient's fever or infection of unknown origin. This procedure may also be used to monitor the progression of a disease, the effectiveness of treatment, and to determine the stage of cancer.
3. How To Prepare

Most individuals will undergo their bone marrow biopsy on an outpatient basis. A bone marrow biopsy is usually performed by a physician who specializes in blood disorders, called a hematologist, or an oncologist, who is a doctor that specializes in cancer. Some patients will be able to undergo this procedure under local anesthesia, while others may choose to have intravenous twilight sedation. Should intravenous sedation be used, the patient should not consume any fluids or food for at least eight hours before the time of their bone marrow biopsy. An individual who decides to have intravenous sedation will need to arrange for a ride to and from the facility where the procedure will be carried out. The physician performing the bone marrow biopsy should be made aware of all medications and supplements the patient takes regularly. An individual who takes antiplatelets, anticoagulants, or nonsteroidal anti-inflammatory drugs regularly will need to stop taking them several days before their bone marrow biopsy to reduce the risk of excessive bleeding.
4. How The Procedure Works

A bone marrow biopsy is usually performed by a hematologist, a doctor with expertise in blood disorders, or an oncologist, a doctor who specializes in cancer. The physician performing the bone marrow biopsy will choose a place to extract the sample tissue from the bone and clean the site with alcohol or an iodine solution. Lidocaine or another local anesthetic is then injected at the site where the biopsy is to be carried out to reduce pain. A specialized bone marrow biopsy needle is then inserted through the skin and into the patient's bone. This part of the procedure is known to produce pressure. The needle used to carry out a bone marrow biopsy has a hollow center and is pressed further into the bone with a twisting motion to produce a small cylindrical tissue sample. During this part of the procedure, it is common for a patient to feel a sharp pain because local anesthetic cannot penetrate the bone tissues. Depending on the age of the patient undergoing the biopsy and other circumstances, medications may be administered before the procedure for partial or full sedation.
5. Risks Of The Procedure
Every procedure carries risks, and while it is minimally invasive, a bone marrow biopsy is no exception. However, complications that result from a bone marrow biopsy are considered very rare, and less than one percent of all bone marrow biopsy procedures cause significant complications. Individuals who are most at risk for experiencing complications include anyone who has been on blood-thinning medications, has a known bleeding disorder, has allergies to any kind of medical equipment or medications, has an immunosuppressive condition or takes immunosuppressants, has low numbers of platelets, or who are pregnant at the time of the procedure. The most common complications that occur with a bone marrow biopsy include persistent or excessive bleeding following the procedure, the development of a post-procedural infection, moderate pain during or following the procedure, and an allergic or adverse reaction to the equipment or medications used during the procedure.
6. Recovery Process

The recovery process following a bone marrow biopsy is not as intense as most surgical procedures but still requires special care and consideration for about a week. Individuals who received sedation during the procedure will be drowsy for several hours until the medication wears off. The incision site is bandaged up and should be kept in place for twenty-four to forty-eight hours following the bone marrow biopsy. After the bandage is removed from the site, the patient should keep the area dry and clean. The physician will provide specific instructions on bathing and cleaning the area, as well as how often to do so. If a patient needs help with pain management, ibuprofen or acetaminophen may be used, because any medication containing acetylsalicylic acid can increase the chances of bleeding complications. All strenuous activities should be avoided for two days following the procedure. Symptoms such as excessive bleeding, swelling, fever, increased pain, or drainage should be reported to the physician.
7. What Abnormal Results Can Mean

A patient's bone marrow tissues are sent to a laboratory where a pathologist evaluates them underneath a powerful microscope for abnormalities. A bone marrow biopsy tells doctors the count and what types of red blood cells, platelets, and white blood cells are present and their stages of development. The cellularity or quantity of blood cells in comparison to other bone marrow components is also examined. The bone marrow biopsy report usually includes a description of the bone marrow environment appearance and the cells that were seen. Too many of certain types of cells that have been identified in an individual's bone marrow can be indicative of myeloproliferative neoplasms or leukemia. Low numbers of red blood cells and hemoglobin can indicate the patient is affected by some form of anemia, and low numbers of other types of cells can indicate myelodysplastic syndrome. Changes observed in the shape of red blood cells can indicate the patient is affected by myelofibrosis or sickle cell anemia. Doctors usually schedule a follow-up appointment to review any abnormal results.
8. Next Steps To Take

An individual who has had a bone marrow biopsy will meet with the ordering doctor after their procedure to go over the results and schedule any follow-up testing that might be necessary. If a bone marrow biopsy has revealed the patient is affected by anemia, their doctor may need to conduct further tests to check for internal bleeding. A kidney biopsy may be needed to rule out kidney failure, which can cause problems with bone marrow and anemia. If the results of the bone marrow biopsy indicate the patient may have cancer in their blood, their doctor may want to carry out biopsies on other tissues they suspect may also be affected. It is common for a patient to have a lymph node biopsy if blood cancer is suspected or diagnosed after a bone marrow biopsy. An individual affected by a myeloproliferative disorder or cancer may need to undergo a follow-up bone marrow biopsy after a little time has passed to help evaluate the efficacy of their treatment.
9. Alternative Diagnostic Tests
Because a bone marrow biopsy can carry risks and tends to be a painful procedure when intravenous sedation is not used, some patients may want to undergo alternative diagnostic tests. Individuals who have been diagnosed by cancer or another bone marrow disorder may not want to undergo multiple bone marrow biopsies or can be in a physical state where they are unable to undergo follow-up bone marrow biopsy. One method being used as an alternative to a follow-up bone marrow biopsy in myeloma patients uses plasma cells captured from blood samples. This test will allow the doctor to identify the stage of the myeloma, the best drug to treat it, and keep an eye out for signs of recurrence in states of remission. The presence of circulating tumor cells or CTCs in the blood, along with the presence of cell-free DNA, can be used for comprehensive genomic profiling. The combination of both of these components is what makes it possible to extract valuable information that helps with the genetic profiling of a patient's cancer.
10. Alternative Uses For Samples

The bone marrow sample taken from a patient who has had a bone marrow biopsy can be used to carry out other helpful diagnostic tests. FISH or fluorescence in situ hybridization is a test that can find genetic abnormalities or alterations in chromosomes a standard microscopy test may not detect. Flow cytometry is a test a bone marrow sample can be used for that determines if a patient's high white blood cell count is being caused by cancer. A bone marrow sample can also be used for immunophenotyping, a test that allows for the identification of certain types of abnormal cells in a patient's blood, lymph node, or bone marrow sample. Karyotype tests, which involve mapping out an individual's 46 chromosomes, their pattern, shape, number, and size can also be carried out on a bone marrow sample. A bone marrow sample can also be used to carry out a polymerase chain reaction test that can detect any cancerous cells in the blood not detected using FISH. Cytogenetic analysis, which is used to detect multiple myeloma, can be carried out on a bone marrow biopsy sample.
11. The Role of Patient Comfort: Beyond Anesthesia

While local anesthesia is standard, the psychological aspect of a bone marrow biopsy is often overlooked. Beyond the numbing agent, many facilities employ comfort techniques like guided meditation, calming music, or even virtual reality to distract and relax patients. Understanding that providers are increasingly focused on holistic comfort – addressing anxiety as much as physical pain – can be a surprising reassurance, making the procedure less daunting for even the most apprehensive individuals.
12. The "Crunch" and "Suck" Sensations

Patients are often warned about "pressure," but the distinct sensations during a bone marrow biopsy can still be surprising. As the needle enters the bone, a deep, grinding "crunch" might be felt. During the aspiration, a unique, fleeting "suck" or tugging sensation occurs as the liquid marrow is drawn. Knowing these specific, odd feelings beforehand can help manage expectations, confirming they are normal parts of the process, not signs of something wrong.
13. Why the Hip (Iliac Crest) is Preferred

While all bones contain marrow, the posterior iliac crest (the back of your hip bone) is overwhelmingly chosen for biopsies. This isn't arbitrary. It’s because this site offers a large, easily accessible bone surface that’s relatively close to the skin, minimizing the risk of hitting vital organs. It also contains abundant active red marrow, yielding a high-quality, representative sample, making it the anatomical sweet spot for diagnostic accuracy.
14. The Small Size of the Sample: A Tiny Window

Despite the invasive nature, the actual bone marrow sample is remarkably small—often just a 1/2 to 1-inch cylindrical piece of bone and a few milliliters of liquid. This tiny amount is astonishingly powerful. This microscopic "window" provides comprehensive information about your blood cell production, cancer presence, or bone marrow health, underscoring the incredible diagnostic precision derived from such a minimal extraction.
15. Pathologist's Eye: More Than Just Cells

The pathologist examining your sample isn't just counting cells; they're interpreting an entire ecosystem. They meticulously assess the "cellularity" (how much marrow is blood-producing vs. fat), the arrangement of cells, presence of abnormal structures, and even the surrounding bone matrix. This holistic evaluation goes beyond simple numbers, providing crucial context for diagnosis and disease classification that a standard blood test cannot offer.
16. Immunophenotyping: Pinpointing Cell Types

Beyond basic cell counts, immunophenotyping is a sophisticated analysis performed on bone marrow samples. This technique uses antibodies to identify specific proteins (markers) on the surface of cells. This allows pathologists to precisely classify abnormal cells, like distinguishing between different types of leukemia or lymphoma, providing critical information for accurate diagnosis, prognosis, and tailored treatment plans that target specific cell characteristics.
17. Cytogenetics and FISH: Unmasking Genetic Faults

Bone marrow biopsies are crucial for uncovering hidden genetic abnormalities. Cytogenetics involves analyzing chromosomes for structural or numerical changes, while FISH (Fluorescence In Situ Hybridization) uses fluorescent probes to detect specific gene mutations or deletions. These tests are vital for diagnosing certain blood cancers (e.g., CML, MDS) and predicting disease progression or treatment response, revealing deep genetic insights invisible through routine microscopy.
18. The "Dry Tap" Phenomenon

Occasionally, during the aspiration part of the biopsy, no liquid marrow can be drawn – this is known as a "dry tap." While it can be frustrating, it's not always a cause for alarm. It can indicate a condition like myelofibrosis (where marrow is replaced by scar tissue), or simply a technical difficulty. Even in a dry tap, the solid core biopsy still provides invaluable diagnostic information, demonstrating the procedure's robust adaptability.
19. Managing Post-Procedure Soreness: Beyond Ibuprofen

While strenuous activity is restricted, lingering soreness at the biopsy site is common. Beyond ibuprofen or acetaminophen, surprisingly, applying an ice pack for the first 24 hours, followed by warm compresses, can significantly reduce localized pain and swelling. Gentle movements, like short walks around the house, can also improve circulation without straining the area, aiding recovery and minimizing stiffness in the days following the procedure.
20. Importance of Follow-Up Biopsies (Monitoring Treatment)

Bone marrow biopsies aren't just for initial diagnosis. For certain conditions, particularly blood cancers like leukemia or multiple myeloma, follow-up biopsies are crucial. These "repeat performances" help oncologists monitor disease progression, assess the effectiveness of chemotherapy or other treatments, and detect remission or relapse. While daunting, these subsequent biopsies provide essential real-time insights guiding critical treatment decisions, ensuring the best possible patient outcomes.
Beyond the Fear

The bone marrow biopsy, once a mysterious and intimidating procedure, is now demystified. We've navigated its 21 surprising twists and turns, from the crucial pre-procedure steps to the intricate lab analyses that unlock vital health insights. You've learned about the unexpected sensations, the tiny yet powerful samples, and the sophisticated genetic tests that reveal hidden truths. Armed with this comprehensive understanding, you can transform apprehension into empowerment. This isn't just a diagnostic tool; it's a profound window into your body's most fundamental processes, guiding precise diagnoses and effective treatments. Step forward with confidence, knowing you are fully informed on this essential journey to understanding and reclaiming your health.
