How to Treat Catecholaminergic Polymorphic Ventricular Tachycardia
Catecholaminergic polymorphic ventricular tachycardia is a rare cardiac condition that causes the heart to beat irregularly and abnormally fast. The disorder is genetic and develops due to mutations on the RYR2 or CASQ2 gene. While this type of ventricular tachycardia can be treated, it is linked with an increased risk of sudden cardiac death. Symptoms of this ailment typically present during childhood, and most patients are seven or eight years old at the time of diagnosis. Catecholaminergic polymorphic ventricular tachycardia is very difficult to detect, and it may go unrecognized even by cardiologists. The earliest symptom is usually fainting (syncope), and patients may also experience dizziness and lightheadedness. The symptoms usually appear with exertion.
Physicians can do genetic tests to diagnose this condition, and these may be recommended for immediate and extended family members of patients with this disorder. Doctors will also perform a physical examination and additional tests, which include listening to the heartbeat to identify abnormal sounds, rates, or rhythms and doing an electrocardiogram to get more detailed information about a patient's cardiac rhythm. Some patients may have a continuous electrocardiogram recording for twenty-four hours. Other tests used to diagnose Catecholaminergic polymorphic ventricular tachycardia include an echocardiogram, an exercise stress test, and MRI scans of the heart.
The following steps are some of the most common treatments for patients with catecholaminergic polymorphic ventricular tachycardia.
Treatment Through Medication

The first line of treatment for catecholaminergic polymorphic ventricular tachycardia is treatment through medication. Patients with the condition will typically be prescribed beta blockers, which need to be taken daily, and work by slowing the heart rhythm and preventing the development of an irregular heartbeat. Examples of common beta blockers include acebutolol, propranolol, atenolol, bisoprolol, nebivolol, and metoprolol. Potential side effects include depression, cold hands and feet, fatigue, weight gain, shortness of breath, and trouble with sleeping. Beta blockers should not be used by patients who have asthma. Patients with catecholaminergic polymorphic ventricular tachycardia who cannot use beta blockers or who need additional medication may need calcium channel blockers. These drugs stop calcium from entering the blood vessels of the heart, and this reduces blood pressure. Calcium channel blockers for this particular condition also slow the heart rate and regulate heart rhythm. Examples of calcium channel blockers include felodipine, isradipine, diltiazem, amlodipine, and nicardipine. Like beta blockers, these are taken daily. Possible side effects include constipation, headaches, rash, fatigue, nausea, and palpitations.
Keep reading for more on how to treat catecholaminergic polymorphic ventricular tachycardia.
Sympathetic Denervation
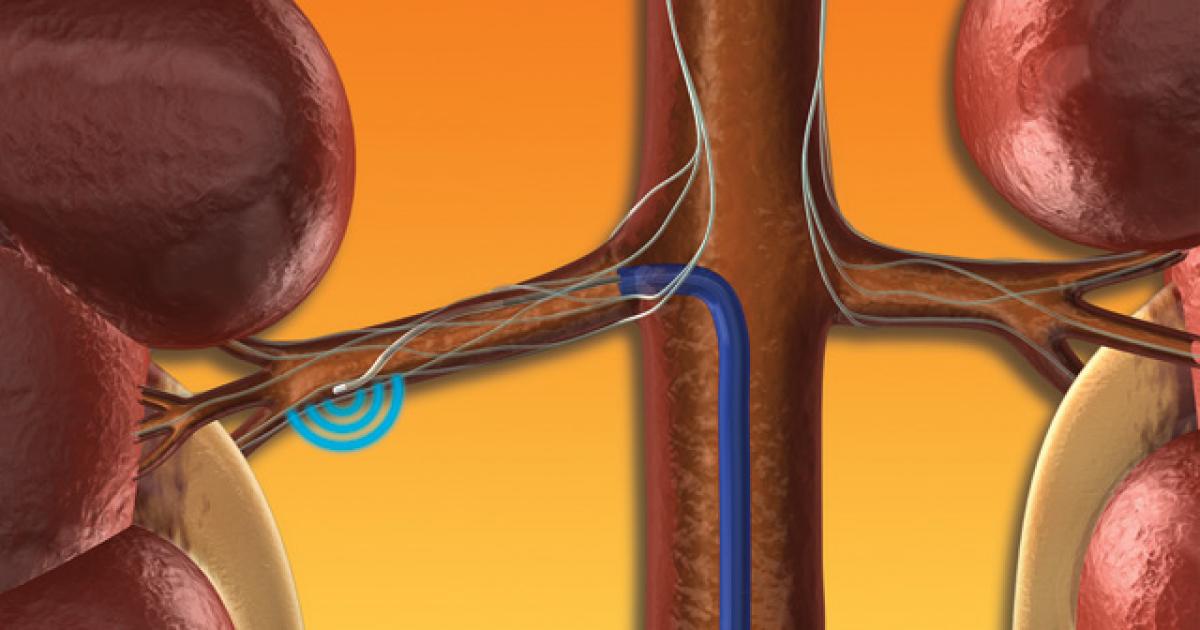
A surgical procedure known as left cardiac sympathetic denervation may be appropriate for patients who experience intolerable side effects from medication. This procedure is also recommended for patients who cannot control their symptoms through other methods. Sympathetic denervation involves removal of the nerves that supply adrenaline, a hormone that tells the heart to beat more quickly. This can reduce episodes of fainting and other symptoms caused by catecholaminergic polymorphic ventricular tachycardia. The procedure is performed under general anesthesia, and surgeons may use videoscopic equipment to assist them during the operation. The surgery usually lasts around forty minutes, and patients will be closely monitored with follow-up appointments. Before the procedure, patients will have a pre-op appointment, which may include a physical exam and tests such as an electrocardiogram.
Learn more about methods of treating catecholaminergic polymorphic ventricular tachycardia now.
