Guide To Treating Chronic Pancreatitis
Chronic pancreatitis is a progressive disease of the pancreas and causes the pancreas to lose its function and structure permanently. The pancreas is found in the abdomen, below the ribcage, and behind the stomach. It is responsible for the production of various hormones and enzymes required for the proper digestion of foods. The pancreas produces insulin or a hormone that regulates and manages the levels of glucose in an individual's blood. Chronic pancreatitis is most often the result of repeated occurrences of acute pancreatitis, which happens when there is premature activation of trypsin in the pancreas. Trypsin is a digestive enzyme that is meant to stay inactive until it reaches the small intestine. In acute pancreatitis, trypsin activates and begins to digest the pancreas itself. This mechanism results in chronic irritation and inflammation of the pancreas that damages it and causes chronic pancreatitis.
Get the details on treating chronic pancreatitis now.
Pancreas Resection

Severe cases of chronic pancreatitis may require a patient to undergo a pancreas resection to treat severe chronic pain. The head of the pancreas becomes severely inflamed and causes the patient to experience intense pain. In a pancreas resection, the pancreas head is removed to alleviate the inflammatory pain irritating the endings of the nerves. A pancreas resection also decreases any pressure on the ducts.
There are three primary methods used for a pancreas resection. The Beger procedure is a method where the head of the pancreas is removed, and the duodenum is spared. The remaining portion of the pancreas is then attached to the intestine. The Frey procedure is a method intended for patients experiencing pain from blocked ducts and an inflamed pancreatic head. The head of the pancreas is removed, and the ducts are attached directly to the intestines to decompress them. A pylorus-sparing pancreaticoduodenectomy is a type of resection that involves the removal of the ducts, gallbladder, and pancreas. This procedure is reserved for the most severe cases of chronic pancreatitis where the ducts are blocked, and the pancreatic head is very inflamed.
Learn more about how to treat chronic pancreatitis now.
Endoscopic Stent Replacement
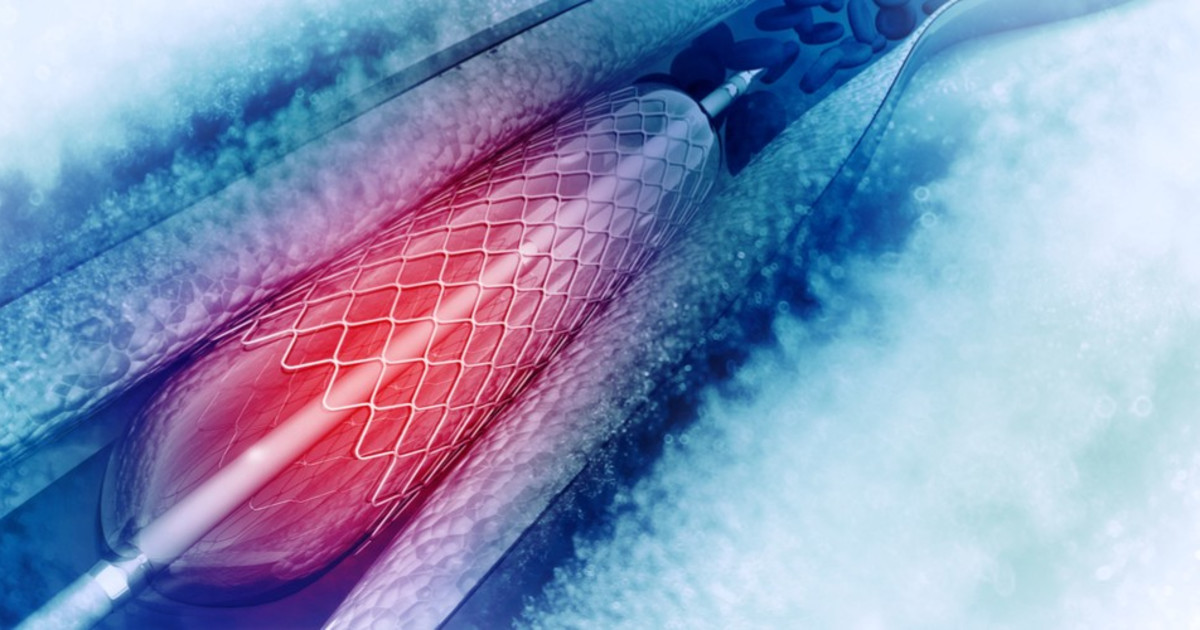
An accumulation of digestive juices in the pancreas may put pressure on ducts that have become blocked, resulting in intense pain. When the pain a patient is experiencing is caused primarily by this mechanism, an endoscopic stent replacement procedure may be needed. This procedure involves the use of ultrasound technology to help guide the surgeon operating the endoscope to the blocked duct. Once the endoscope reaches the blocked duct, a balloon catheter is threaded into the endoscope and to the duct. The surgeon then inflates the balloon on the end of the catheter inside of the duct, effectively widening it. A medical mesh stent is then placed into the duct around the balloon to hold it open. The balloon is deflated, and the stent is left in the duct to prevent it from becoming narrowed again. An endoscopic stent replacement surgery is minimally invasive and carries less risk of complications than traditional open procedures used to widen ducts.
Discover more treatment methods for chronic pancreatitis now.
