The Dangers Of Deep Vein Thrombosis
Deep vein thrombosis, also known as thromboembolism and postphlebitic syndrome, is a critical and sometimes fatal blood condition that occurs when blood clots form in various parts of the body, typically in a leg or the lower half of the body. There are specific signs and symptoms patients need to be aware of, especially if they are at high risk of developing blood clots due to genetics or their lifestyle. Start reading to discover what causes this severe condition, its symptoms, the fatal complications it can lead to, and how individuals can prevent it.
What Is Deep Vein Thrombosis?
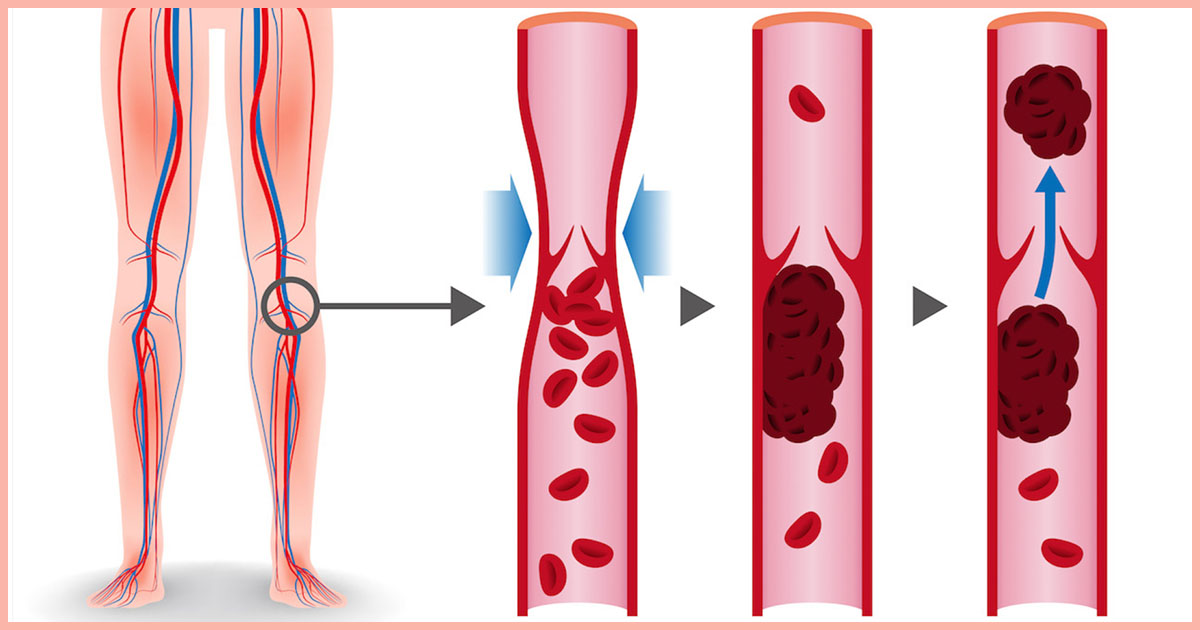
Deep vein thrombosis, also known as DVT, occurs when a thrombus, commonly called a blood clot, forms in one or more of the deep veins within the body, particularly in the legs, thighs and lower extremities, though it can also occur in other parts of the body. A blood clot is a clump of blood in a gelatinous, solid state that blocks blood from flowing freely due to its size. This condition can result in leg pain or swelling, however, it is common for a patient to not experience noticeable symptoms, and DVT will only become apparent once a pulmonary embolism occurs. Deep vein thrombosis can become severe and even fatal, as the blood clots in the veins may break loose, travel through the bloodstream, and become embedded in the lungs, blocking blood flow, resulting in a pulmonary embolism.
Signs & Symptoms To Be Aware Of

Typical symptoms and signs of deep vein thrombosis include swelling and acute pain in the affected leg that often starts in the calf and can feel like cramping or tenderness, red or discolored skin in the affected area, and a feeling of intense warmth in the affected area. According to the National Heart, Lung, and Blood Institute, additional common symptoms include swelling of a foot or ankle, and severe, unexplained pain in the foot and ankle. These symptoms usually only occur in about half of the individuals who have the condition, as the other half does not show any visible signs.
What Causes DVT?

The blood clots of deep vein thrombosis can be caused by anything that prevents blood from flowing freely throughout the body and clotting normally, such as an injury to a vein, surgery especially on the lower extremities, specific medications, and limited movement. One of the most predominant risk factors for developing DVT is if a patient inherits a blood-clotting disorder that allows their blood to clot more easily. However, the inherited condition might not cause blood clots alone unless it is combined with one or more risk factors.
Risk Factors Patients Need To Be Aware Of

Prolonged bed rest or limited movements, such as during an extensive hospital stay or paralysis can result in DVT. This is especially true for the legs as if they remain still for long periods, the calf muscles do not contract properly to help blood circulate, increasing the chances of the formation of blood clots. Pregnancy increases the risk factor of a woman developing DVT, as it increases pressure on the woman's veins in the pelvis and legs, and the risk is still present for up to six weeks after giving birth. Other risk factors include birth control pills and other oral contraceptives, hormone replacement therapy, some forms of cancer, heart failure, inflammatory bowel disease, a patient over the age of sixty, heavy smoking, and being overweight or obese.
Complications Associated With DVT

One of the scariest and occasionally fatal complications of DVT is the patient developing a pulmonary embolism. As previously mentioned, a pulmonary embolism occurs when a blood clot travels to the lung from another area of the body, typically from the leg, and blocks a blood vessel in the lung. A pulmonary embolism can be life-threatening, and it is essential for a patient to be aware and watch for its signs and symptoms and seek medical attention immediately if they notice any of them. Signs and symptoms of a pulmonary embolism include sudden shortness of breath, chest pain or discomfort that worsens when a patient takes a deep breath or coughs, experiencing dizziness or fainting, a rapid pulse, and coughing up blood.
Another common complication associated with DVT is postphlebitic syndrome, which occurs after DVT and is when the veins become damaged from the blood clot and decrease blood flow in the affected areas. Signs and symptoms of this complication include persistent swelling of the legs, known as edema, leg pain, skin discoloration and skin sores.
When To See A Doctor

Deep vein thrombosis is a serious medical condition that should be closely monitored and prevented at all costs. Individuals who have a family medical history of blood disorders and blood clotting may inherit these disorders, and thus should visit their doctor frequently, especially if they experience one or more of the risk factors, such as if they are overweight or smoke.
If an individual is experiencing any symptoms of DVT, whether they are at an increased risk or not, should contact their doctor immediately or go to the closest emergency room to prevent further complications, such as a pulmonary embolism. If someone does not believe they have DVT but are concerned they could be at risk for developing the condition, they should schedule an appointment with their doctor, as their doctor can prescribe preventive treatment if necessary.
Prevention Tips

There are a few options individuals have when it comes to preventing deep vein thrombosis from happening to them. One of the primary ways to prevent this disorder is for a patient to avoid sitting still and to keep moving as much as possible, especially after surgery or if they have been put on bed rest. If an individual has been sitting for awhile, such as while driving or on a flight, do not cross the legs, which can decrease blood flow, and if traveling, try to move around as much as physically possible.
Another great preventative measure an individual can take is to make lifestyle changes, such as losing weight if overweight and to quit smoking, as both increases a patient’s risk of developing DVT astronomically. Regular exercise is also recommended as it lowers the risk of developing blood clots within the veins, and exercise is especially necessary for individuals who sit a lot or travel frequently.
Diagnosis & Treatment Options For Patients At Risk

For an accurate diagnosis, a physician will ask patients about their family medical history and the symptoms they are experiencing. The doctor will conduct a physical exam so they can check the affected areas for discoloration, swelling, and tenderness. Depending on the chances of a patient developing deep vein thrombosis or blood clotting, further testing for a diagnosis can include an ultrasound, a blood test, a venography, and a CT or MRI scan. Treatment for DVT is aimed at preventing a blood clot from becoming larger or preventing it from breaking loose and resulting in a pulmonary embolism.
A typical treatment option is for a patient to take anticoagulants, or blood thinners, which can be taken in a pill form or as an injection, and decreases the risk of blood clots. Thrombolytics, known as clot busters, break up blood clots rapidly and are also another common treatment, especially if the patient develops a more severe form of DVT or a pulmonary embolism. Other options for patients is having a filter inserted into a large vein, known as the vena cava, in the abdomen to prevent clots from breaking loose and becoming lodged in the lungs, as well as compression socks, which can be worn for up to two years in some instances, to prevent swelling in the legs. If you or a loved one believe you may be at risk for developing deep vein thrombosis, schedule an appointment with a doctor to review preventative measures you can take and to ensure you receive the best possible treatment.
