Methods Of Treating And Preventing Hyponatremia
Hyponatremia is the medical term for low sodium in the blood. This condition is very common, and individuals in their sixties and beyond face an increased risk of developing it. In some cases, the severity of hyponatremia may be mild, but it can be a life-threatening condition for some patients. The disorder can be caused by underlying medical conditions and by drinking too much water. Patients who suspect they have hyponatremia should see their healthcare provider for a physical exam and laboratory tests. During the physical exam, doctors will examine the patient's cardiovascular and gastrointestinal systems. Patients will be asked questions about their medications, mood, bowels, and energy levels. Blood and urine tests are needed to diagnose hyponatremia, and it is typically brief, lasting days or weeks rather than months. Symptoms of low sodium in the blood generally include nausea, fatigue, confusion, irritability, muscle cramps, and headaches. In more severe cases, patients may experience seizures and even become comatose. The methods outlined below are useful in the prevention and treatment of hyponatremia.
Reduce Fluid Consumption

While it's crucial to be properly hydrated, patients at risk for hyponatremia need to be mindful of their fluid consumption. The two liters of water recommended per person each day by the World Health Organization and even the eight glasses of water recommended by other experts may be too much for some individuals. Instead of going solely by these numbers, patients should use their urine color and sense of thirst as guidelines. Patients who do not feel thirsty and who have pale yellow urine are likely sufficiently hydrated. Athletes and individuals participating in endurance sports such as marathons may need to reduce fluid consumption before, during, and after these intense activities. Rather than binging on water and sports drinks, they should aim to drink only as much fluid as they lose through sweat during exercise.
Get the details on the next method of treating hyponatremia now.
Intravenous Sodium Solution
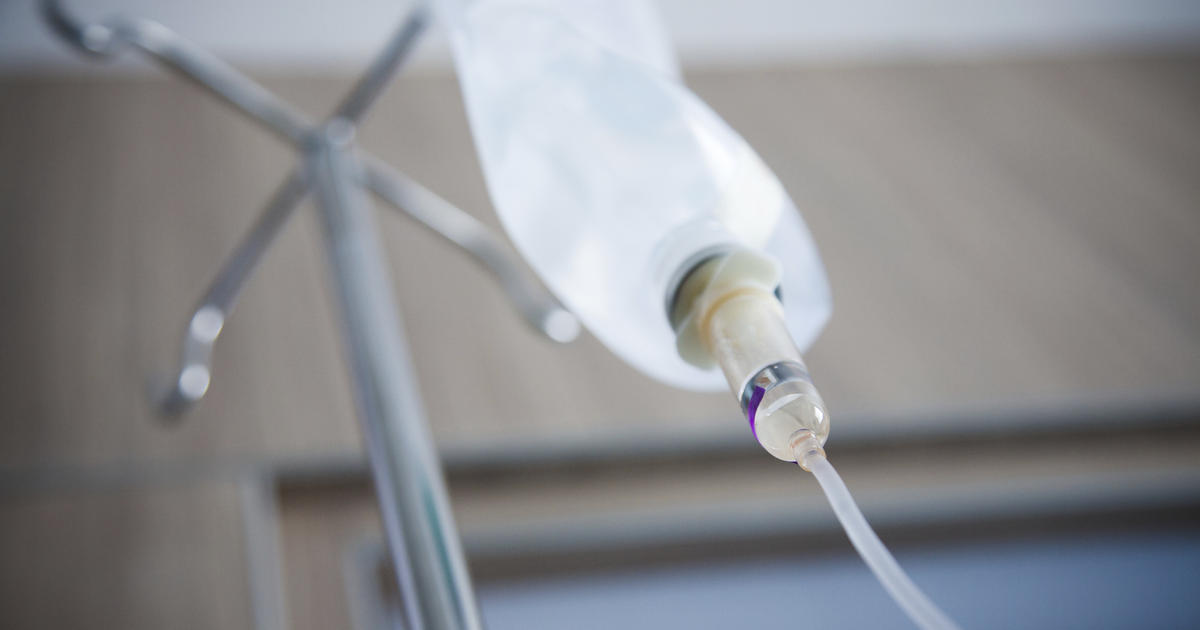
In cases of acute or severe hyponatremia, an intravenous sodium solution may be needed to raise sodium levels back to normal. Doctors must raise the level of sodium in the patient's blood slowly to avoid serious complications. Patients must be admitted to the hospital to receive the intravenous sodium solution, and they will have frequent blood tests to monitor their sodium levels as the treatment is being given. Typically, treatment takes at least one day in the hospital. While at the hospital, patients will have their blood pressure, heart rate, and temperature measured regularly, and they will be connected to an electrocardiogram machine to provide a continuous recording of cardiac output. As the treatment is administered, patients should report any changes in their condition to a member of their hospital team.
Reveal more treatments for hyponatremia now.
Medication For Symptom Management

Hyponatremia can cause a range of symptoms depending on the severity of the condition, and medication for symptom management is often recommended. Headaches are among the most common symptoms, and these can be relieved by taking over the counter medications such as ibuprofen. If patients cannot get relief from their headaches with these medicines, doctors may prescribe stronger ones. Nausea and vomiting may occur with hyponatremia, and these are most effectively managed with medications such as ondansetron, dexamethasone, diphenhydramine, and dimenhydrinate. Hyponatremia can cause seizures, which are typically managed with injections of lorazepam and other anticonvulsants such as lamotrigine, levetiracetam, and gabapentin, in the most severe cases. Patients taking any of these medications will be closely monitored for side effects and changes in their health, and regular blood tests may be needed while taking certain medicines. Patients should report any new or worsening symptoms to their healthcare providers.
Keep reading to learn about more ways to treat hyponatremia now.
Monitor Use Of Diuretics

Diuretics come in three major types, and they are often used as the first line of treatment for high blood pressure. They are also used to treat congestive heart failure, a disease that affects how well the heart pumps, and edema, a condition that results in swelling in the lower limbs and feet. Some examples of thiazide diuretics, the most commonly prescribed form, include chlorothiazide, chlorthalidone, hydrochlorothiazide, and metolazone. Loop diuretics, used in the treatment of heart failure, include torsemide, furosemide, and bumetanide. In patients at risk of potassium imbalances, doctors typically prescribe potassium-sparing diuretics. These include amiloride, spironolactone, triamterene, and eplerenone. Doctors often monitor use of diuretics in older patients to reduce their risk of sodium imbalances. The medication works by increasing water and salt expelled from the body through urination, and this can occasionally cause hyponatremia.
Diuretics are usually taken by patients at least once a day, and they can cause side effects. Depending on the type of diuretic used, side effects generally include increased cholesterol, rashes, muscle cramps, headaches, diarrhea, increased blood sugar, high potassium, and feeling thirsty. Very rarely, diuretics can trigger arrhythmias and kidney failure. Patients on these medications may need to have their kidney function monitored with blood tests, and their cardiac health may also need to be examined regularly.
Get familiar with the next option for treating hyponatremia now.
Treating Associated Illness

Hyponatremia may sometimes develop as the result of an underlying medical condition. Treating associated illness can help reduce the symptoms of hyponatremia and allow the patient to make a full recovery. Congestive heart failure and diseases of the liver and kidneys are the most common medical conditions associated with hyponatremia. Addison's disease is another cause of low sodium in the bloodstream. This condition, also known as adrenal gland insufficiency, occurs when the adrenal glands cannot effectively produce the hormones needed to maintain sodium levels in the body. A rare disorder known as the syndrome of inappropriate anti-diuretic hormone is also linked to the development of hyponatremia. The condition causes the body to produce too much of the anti-diuretic hormone, and the body then retains water instead of getting rid of it through urination. Occasionally, treating depression with antidepressants may cause patients to develop hyponatremia. The most effective treatments for these underlying conditions vary, and patients with these health issues or any other conditions should consult their doctors for personalized treatment recommendations.
