A Comprehensive Guide To Sickle Cell Anemia
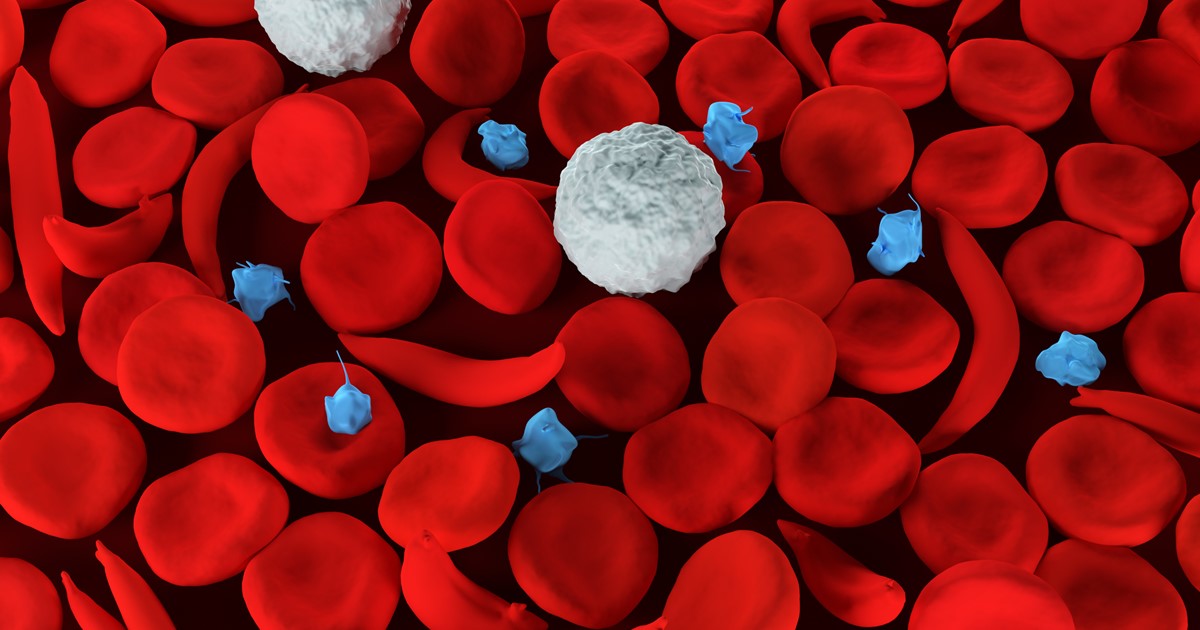
Sickle cell anemia, also known as sickle cell disease, is a common genetic disorder that affects the red blood cells and is an inherited form of hemolytic anemia, said to be more prevalent in African American individuals. It is a condition in which there are not enough healthy red blood cells to carry adequate oxygen throughout the body and to all of its vital organs. The sickled red blood cells are fragile and can rupture quite easily, hence when the amount of healthy red blood cells decrease from a rupture. This is known as hemolysis and results in anemia.
Learn how this genetic blood disease develops, the specific genetic trait that causes it, the symptoms individuals endure when afflicted with this incurable disease, along with other details such as treatment options and prognosis. Let's start with learning what the sickle trait is and how it is passed on through generations.
What Is The Sickle Trait & How Is It Passed On?

Sickle cell anemia is inherited as an autosomal, meaning the gene that causes this disease is not linked to sex chromosomes and is a recessive condition. The gene containing the DNA for this condition can be passed on from one parent who is a carrier to a child. For sickle cell anemia to manifest a sickle cell gene must be inherited from both the mother and father, so the child has two sickle cell genes. If a child only inherits one gene, this is called the sickle cell trait or the carrier state, as the sickle cell trait does not cause sickle cell anemia. Carriers often do not experience any of the symptoms those affected by the disease do. However, when two carriers of the sickle cell trait produce offspring, their children have a one in four chance of developing sickle cell anemia.
What is the sickle cell trait specifically? It begins with the red blood cells manufactured in the bone marrow and their complex biconcave shape expand, so they have adequate storage capacity for hemoglobin molecules that carry oxygen throughout the body. This makes the cells soft and flexible so they may squeeze through incredibly tiny blood vessels in the body. However, in sickle disease and with the trait, these red blood cells form an abnormal crescent shape and can no longer fit into these tiny spaces, which increases the chance of the patient developing blood clots in small capillaries of different organs and leads to organ damage.
Get the major details on the main types of sickle cell anemia now.
Main Types of Sickle Cell Anemia
There are a few main types of sickle cell anemia. The most common and severe type is hemoglobin SS disease. The second most common type is hemoglobin SC, which has similar symptoms to hemoglobin SS with less severe anemia. Hemoglobin SB+ thalassemia is a type of sickle cell anemia that occurs when beta-globin gene production is affected, and red blood cells are smaller because of the reduced amount of beta protein. The symptoms aren't as severe as with the first two types. Sickle beta-zero thalassemia has similar symptoms to SB+ thalassemia and has the same cause, but the symptoms are more severe. Hemoglobin SD, SE, and SO are rare forms of sickle cell anemia and don't tend to have severe symptoms.
Continue reading to learn about the symptoms a patient should be aware of if they believe they might have sickle cell anemia.
Symptoms To Be Aware Of

All of the significant symptoms patients with sickle cell anemia experience are a direct result of the abnormally shaped, sickled red blood cells that block blood flow from circulating throughout the tissues of the body. Due to impaired circulation, these tissues suffer great damage from a lack of oxygen and patients who suffer from extensive tissue and organ damage can experience severe disability and a lower quality of life. As a result of this impairment, patients endure episodes of pain known as ‘crises’ that vary in frequency and severity, depending on the degree of the organ involved.
The predominant symptoms include fatigue and anemia, pain crises, swelling and inflammation of the hands and feet known as dactylitis, arthritis, bacterial infections, splenic sequestration, liver congestion, lung and heart injury, and leg ulcers. Other symptoms include aseptic necrosis and bone infarcts, eye damage, and additional features, such as the weakening of the bones due to osteoporosis, kidney damage and infection, and nervous system damage. It should be noted symptoms can occur at any age, however, specific symptoms can appear for specific age groups.
Keep reading to discover the causes of sickle cell anemia and how not just genetics, but specific organs, can play an important role.
What Are The Causes?
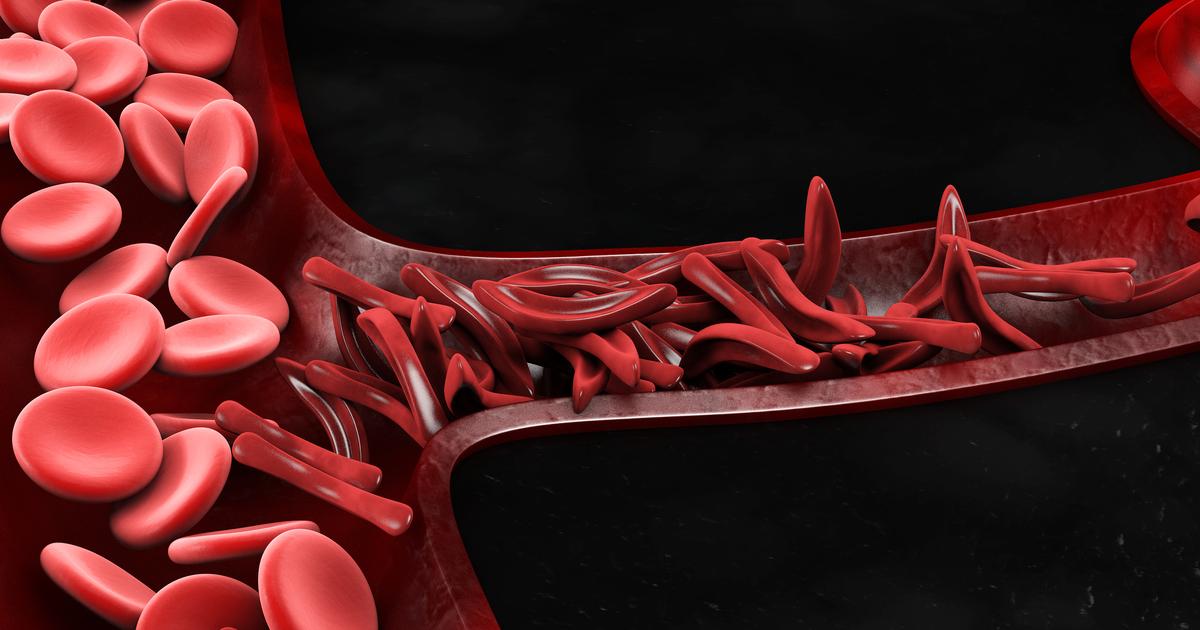
Considering we know what sickle cell trait is and how it occurs, how does it develop into sickle cell anemia? To begin, the sickling of the red blood cells are a result of the cells becoming abnormal shapes (such as resembling crescents) and diminished flexibility often promoted by conditions associated with low oxygen levels, increased acidity, or lower blood volumes within the body. These conditions for the sickling of the cells to occur can be the result of an injury to the body’s tissues, dehydration, or anesthesia. Specific organs predisposed to lower oxygen levels or acidity are the liver, kidneys, and spleen, as well as organs with high metabolism rates, such as the brain, muscles, and in the placenta of a female who is pregnant and has the condition. In addition to inheriting the sickle trait, these conditions promote the sickling of the cells as these factors extract more oxygen from the blood, making these vital organs susceptible to injury from sickle cell anemia.
As mentioned earlier, specifically with sickle cell anemia, the red blood cells form a rigid crescent shape that results in damage to red blood cells and often leads to blood clots and organ damage. The main cause of sickle cell anemia is inherited abnormal hemoglobin, which is the protein that carries oxygen from the lungs to the body’s tissues and returns carbon dioxide from the tissues back to the lungs. This abnormal hemoglobin protein is what causes distorted or sickled red blood cells.
Learn about the groups most at-risk of developing sickle cell anemia now.
At-Risk Groups

As stated, sickle cell anemia is an inherited disease caused by a genetic mutation, and as such, individuals with a family history of the illness are at a larger risk of having it or passing it on to their offspring. Additionally, most sickle cell anemia patients in the United States are black. Around eight percent of African American individuals have the illness, and one in twelve African Americans carries some form of the sickle cell trait. The disease is also seen in Latino Americans from South and Central America. In addition, individuals of Mediterranean, Indian, Asian, and Middle Eastern descent are at a slightly higher risk of the disease.
Get the details on potential complications linked to sickle cell anemia now.
Serious Complications of Sickle Cell Anemia

The first complication linked to sickle cell anemia is swelling of the feet and hands, often caused by blood flow being blocked out of the appendages. The most commonly experienced complication is pain, which is the main reason most patients with sickle cell anemia need to be hospitalized. Acute chest syndrome, another complication, is a potentially life-threatening condition that presents with difficulty breathing, fever, coughing, and chest pain. Another potentially life-threatening condition is splenic sequestration, which occurs when a large number of sickle cells become trapped in the spleen, causing sudden enlargement of the spleen. If blood cells in the eye become blocked by sickle cells, patients may partially or totally lose their vision. Leg ulcers may also occur on the lower portion of the leg. If blood flow to the brain is blocked, sickle cell anemia patients may have a stroke.
Still curious? Find out how sickle cell anemia is diagnosed next.
How Is It Diagnosed?

Sickle cell anemia can be diagnosed in a few different ways. One way is the abnormal sickle-shaped cells in the blood can be identified under a microscope, where a smear of blood is extracted and tested using a special low-oxygen preparation known as a sickle prep. Other prep tests can also identify the abnormal hemoglobin in the blood, including solubility tests performed on vials of blood solutions. The disease can be determined by quantifying the types of hemoglobin present using hemoglobin electrophoresis, which precisely identifies the hemoglobins in the blood by separating them. This is made possible due to the unique electrical charges each hemoglobin has on their protein surfaces. Prenatal diagnosis can also occur before birth if the mother suffers from sickle cell anemia, or is at least a carrier, by using amniocentesis or chorionic villus sampling. The sample obtained from the womb is then tested for DNA analysis of the fetal cells.
Keep reading to unearth the variety of treatment options available to patients dealing with the disease.
Available Treatment Options

There is no cure for sickle cell anemia, but there are numerous treatment options that can manage and prevent the condition based on the individual features of the illness present. Treatments are directed at the management and prevention of the red blood cells from stacking on top of each other, which forms blood clots. It is essential for affected individuals to have a profound understanding of the disease and to communicate with medical professionals to ensure they are receiving the proper care for the symptoms they exhibit. However, sickle cell anemia tends to become stable without specific treatments over time. Treatment options also depend on the degree of anemia the patient has, which is defined by their blood hemoglobin level.
One treatment option is a blood transfusion, which is required when a severe drop in hemoglobin occurs to correct the anemia and also for patients who are dealing with other complications such as pneumonia, lung infarction, stroke, leg ulcers, or late pregnancy. A transfusion can remove some of the sickle blood cells and replace them with healthy blood cells. Hydroxyurea is a medication that can also be used for adults and children who suffer from severe pain associated with the illness, as well as for individuals who have recurrent strokes and frequent transfusions. The drug increases the amount of fetal hemoglobin in the blood, a form of the molecule resistant to the sickling of the red blood cells found in infants right after birth.
Understand the role of stem cell transplants in sickle cell anemia treatment next.
Use Of Stem Cell Transplants

In recent years, the use of stem cell transplants has shown promise as a treatment method for various conditions, including sickle cell anemia, though more research needs to be done to determine its efficacy. In one study, adults with severe sickle cell anemia received successful treatment through a stem cell transplant. They didn't need extensive immunosuppressants afterward. In addition, multiple children have received successful treatment through a stem cell transplant. At first, these transplants were deemed unviable for adults, but recent studies indicate they may not be. When children with sickle cell anemia received a stem cell transplant, their bodies showed a mix of the donor's blood cells and their own. Even though there was a mix, there wasn't any sign of sickle cell anemia. These were the findings that led researchers to attempt the transplant process with adults.
Find out what the prognosis and next steps are for sickle cell anemia patients now.
Prognosis

Considering there is no cure for sickle cell anemia, the life expectancy of an afflicted individual is reduced as some individuals may not survive past infancy or early childhood. Although rare, some patients can remain without symptoms for years and not discover the condition until they are an adult. Regardless, with optimal management of the condition patients can survive beyond forty years old and have a somewhat normal life expectancy. The main causes of death for patients with this genetic condition are bacterial infections, a stroke, bleeding of the brain, and heart, kidney, or liver failure. Bacterial infections are the most common cause of death for any sickle cell anemia patient at any age. Therefore, if any signs of infection appear, patients should receive immediate medical attention to prevent any further (organ) damage and to save their life.
Continue to discover information on other types of inherited hemolytic anemia now.
Other Types of Inherited Hemolytic Anemia
Hemolytic anemia is a condition that causes red blood cells to die or be destroyed faster than replacements are made. While sickle cell anemia is the most common type of inherited hemolytic anemia, there are other types as well. These include red cell membrane disorders, pyruvate kinase deficiency, and glucose-6-phosphate dehydrogenase deficiency. With a membrane disorder, the membrane of red blood cells becomes too easily damaged or is incomplete. Pyruvate kinase deficiency, meanwhile, is caused by a mutation in an individual's PKLR gene. This gene creates an enzyme known as pyruvate kinase, which is essential in breaking down glucose to give red blood cells energy. When there isn't enough of this enzyme, the body can't convert enough glucose into energy. G6PD deficiency occurs when the body doesn't produce enough G6PD, an enzyme that makes red blood cells work. This enzyme also protects the cells from substances that could cause them harm.
