Guide To Colon Cancer Causes And Risk Factors
Colon cancer is a malignancy that originates in an individual's large intestine or colon. Colon cancer can develop in an individual of any age but is more common in older adults. Symptoms of colon cancer include changes in stool consistency, frequent diarrhea, frequent constipation, blood in the stool, cramping, abdominal discomfort, excessive gas, the sensation of incomplete bowel emptying, weight loss, fatigue, and weakness. Most individuals who do not have numerous risk factors begin getting screened for colon cancer when they reach the fifth decade of life.
Colon cancer is diagnosed with the use of blood tests, CT scans, and a procedure called a colonoscopy. Should the physician discover any areas that look suspicious during a colonoscopy, they can biopsy the suspicious tissue during the procedure. Treatment for colon cancer includes surgery to remove the malignancy if possible, chemotherapy, and radiation therapy.
Family History Of Colon Cancer

Individuals who have a family history of colon cancer are more likely to develop this type of malignancy in their colon. Malignancy anywhere in the body is caused by a change or mutation in cellular DNA that causes the cells to grow rapidly, multiply excessively, and live longer then they should. Some of the mutations that cause cancer can be inherited from an individual's parents. While this cause of colon cancer is relatively uncommon, specific inherited syndromes like familial adenomatous polyposis and hereditary nonpolyposis colorectal cancer can significantly increase an individual's risk of developing colon cancer.
A patient's chance of developing colon cancer is even higher when they have more than one blood family member who has been affected by colon or rectal cancer at some point in their life. Between five and ten percent of all cases of colon cancer are the result of an inherited genetic factor or syndrome. An individual who has a family history of polyp development in the colon or a condition that causes them is also at an increased risk of developing colon cancer.
History Of Colon Polyps
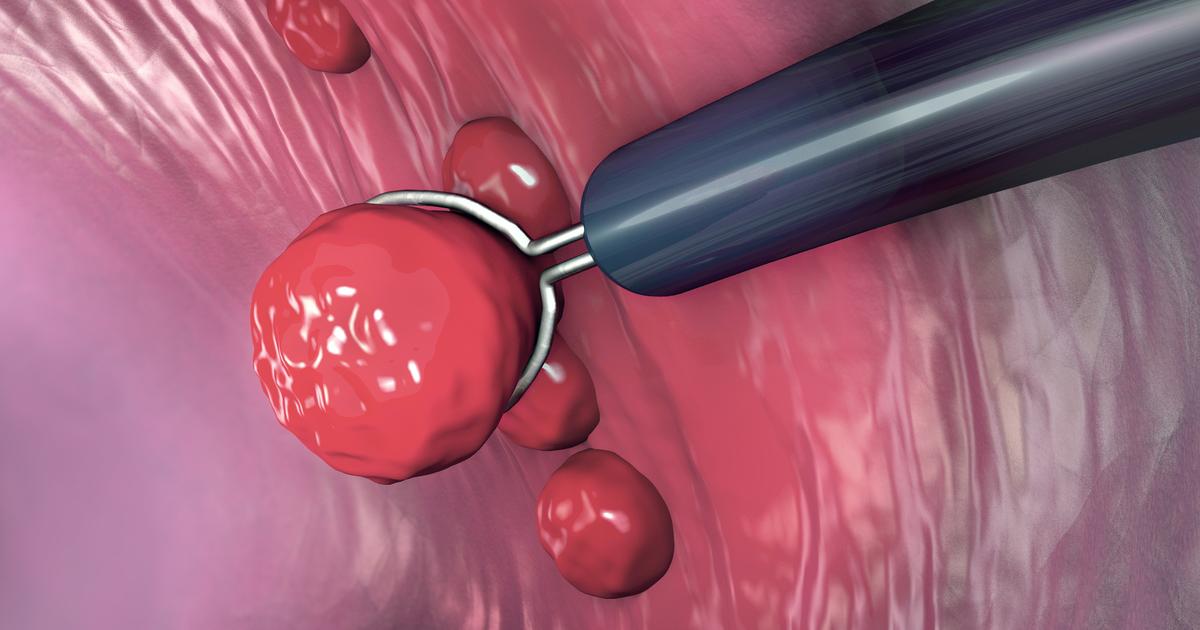
An individual who has a history of colon polyps is at a higher risk of developing colon cancer than an individual who does not. A colon polyp is an abnormal tissue growth that occurs inside of the colon or large intestine. Polyps come in different shapes and sizes. The most common kind of polyp known to increase an individual's risk of developing colon cancer is called an adenomatous polyp. These types of polyps are often associated with mutations in the DNA of cells that make up the large intestine lining.
This malfunction means the larger an adenomatous polyp grows, the more likely it is to incur a DNA mutation that causes the development of colon cancer. Colon polyps can only be found with a procedure referred to as a colonoscopy. Most adenomatous polyps do not produce any symptoms, so most individuals are unaware they have them until they undergo a routine colonoscopy. Colon polyps are removed as soon as they are found to prevent the development of colon cancer.
Sedentary Lifestyle

A sedentary lifestyle can cause an individual to have a higher risk of developing colon cancer than one who has a more active lifestyle. A sedentary lifestyle is best defined as a type of lifestyle will very little or even no physical activity. The exact correlation between a sedentary lifestyle and colon cancer is not clear, but it is thought to be associated with the development of a metabolic disorder, inflammation, and adiposity accumulation.
Other factors can compound the sedentary lifestyle risk factor for colon cancer, such as insulin resistance, altered secretion of adipokines, and increased levels of sex hormones. A sedentary lifestyle also slows down an individual's metabolism and slows the movement of food through their gastrointestinal tract. Slowed digestive motility is known to produce chronic inflammation and intestinal tissue damage, which can increase an individual's risk of developing colon cancer.
Diabetes

A common increased risk factor that implicates a good number of individuals is diabetes, a disease characterized by persistent high blood glucose levels and insulin resistance. An increased risk of colon cancer is associated with type 2 diabetes more than it is with type 1 diabetes. The body produces insulin, but the tissues do not respond to it appropriately in an individual with type 2 diabetes. Individuals with type 2 diabetes often develop chronic compensatory hyperinsulinemia. This type of diabetes has a high correlation with a high-calorie diet, excess abdominal fat, and increased body weight.
Carcinogenesis in type 2 diabetes patients is exacerbated by the interactions of insulin-like growth factor-1. The interaction of the insulin hormone and insulin-like growth factor-1 receptors can prolong cell survival and stimulate the proliferation of cells. Both of these characteristics are important for the formation of malignancy in a patient's tissues. Diabetes also promotes inflammation in the body through several mechanisms, which compounds the risk of developing colon cancer.
Low-Fiber And High-Fat Diet

An individual who primarily lives on a low fiber and high-fat diet is at a higher risk of developing colon cancer than someone who consumes a healthier diet. Fiber is a dietary nutrient known to be essential for optimal colon health. Fiber helps the food move through the gastrointestinal tract faster because it adds bulk to the stools. Fiber is also effective at helping to clean the colon of waste product buildup and bacteria that can cause inflammation. Finally, fiber assists with keeping the bowel movements regular, soft, and healthy. However, all these benefits of fiber are significantly reduced when a low-fiber diet is continuously consumed.
A high-fat diet can help promote the carcinogenesis and growth of malignant cells. Fats are the hardest type of nutrient for the gastrointestinal tract to digest and longer than other nutrients to digest. When an individual consumes a diet full of fatty foods, their liver, pancreas, stomach, and intestines may have trouble producing enough bile acids to metabolize and digest it all properly. This mechanism can cause an imbalance in the intestinal bile acids, which consequently triggers a hormonal response. This hormonal response can promote the growth and proliferation of precancerous and cancerous cells, leading to colon cancer.
Ulcerative Colitis

Ulcerative colitis is a form of inflammatory bowel disease where an individual experiences tissue damage, long-lasting inflammation, and ulcers throughout their digestive tract. Most patients experience the effects of ulcerative colitis in the interior lining of their large intestine. The body is continuously repairing the damage to the tissues and cells that make up the inner intestine lining in an ulcerative colitis patient. This high turnover and repair rate in the intestinal tissues provides more opportunities than usual for a change or mutation to occur in the DNA of the intestinal cells.
A DNA mutation in one of the intestinal cells that causes it to grow rapidly and replicate out of control can cause an individual to develop a growth of malignant cells. When a growth of malignant cells forms in the large intestine, it is referred to as colon cancer. Out of all individuals affected by ulcerative colitis for twenty years or longer, eight percent will develop colon cancer.
Smoking And Alcohol Consumption

An individual who makes certain lifestyle choices will be at an increased risk of developing colon cancer in comparison to someone who makes healthier lifestyle choices. Smoking cigarettes regularly increases an individual's risk of developing hundreds of different types of cancer, including colon cancer. Thousands of toxins in cigarette smoke enter an individual's body when they smoke and can cause damage to the tissues in the digestive tract. This damage to the cells provides greater opportunity for a carcinogenic mutation to occur in the affected area.
Regular and excessive consumption of alcohol can also cause excessive damage to digestive organs and tissues over time. When the body is constantly repairing damage to cells compromised by toxins like those in cigarette smoke and alcohol, there is more opportunity for a mutation to take place. The repair mechanisms in the body are typically able to mediate cellular damage, but mistakes do happen in these processes and can lead to the development of malignancy in the intestinal tissues.
Lynch Syndrome

An individual affected by Lynch syndrome, also called hereditary non-polyposis colorectal cancer, is at an increased risk of developing colon cancer. Lynch syndrome also increases an affected individual's risk for developing other cancers, such as ovarian, stomach, pancreatic, urinary tract, kidney, endometrial, breast, small bowel, prostate, liver, and bile duct cancers. Genetic errors in certain genes, including the MHL1, MSH6, EPCAM, MSH2, and PMS2 genes, are what cause a Lynch syndrome patient to be at a higher risk of developing cancer.
The alterations in the genes that cause Lynch syndrome are inherited. Between three and five percent of all diagnosed cases of colon cancer are thought to be attributed to Lynch syndrome. A simple genetic blood test that detects the aforementioned gene mutations can determine if a patient who has been diagnosed with colon cancer is affected by Lynch syndrome.
Certain Ethnicities

Individuals of certain ethnicities are at a higher risk of developing colon cancer than individuals of other ethnicities. Studies have revealed those of African American descent who live in the United States are more likely to develop colon cancer than Caucasians. Although African Americans in the United States have eighty percent of their genetic material in common with African Americans in Africa, there are substantial differences in the rate of colon cancer development between these populations.
In the United States, between fifty and sixty African Americans develop colon cancer out of every 100,000, where less than five out of every 100,000 in Africa develop colon cancer. It is thought that the higher incidence of colon cancer in African Americans in the United States is attributed to low colon cancer screening rates among this population. Lack of awareness and lack of medical access are both factors that may contribute to the low screening rates among African Americans.
Familial Adenomatous Polyposis
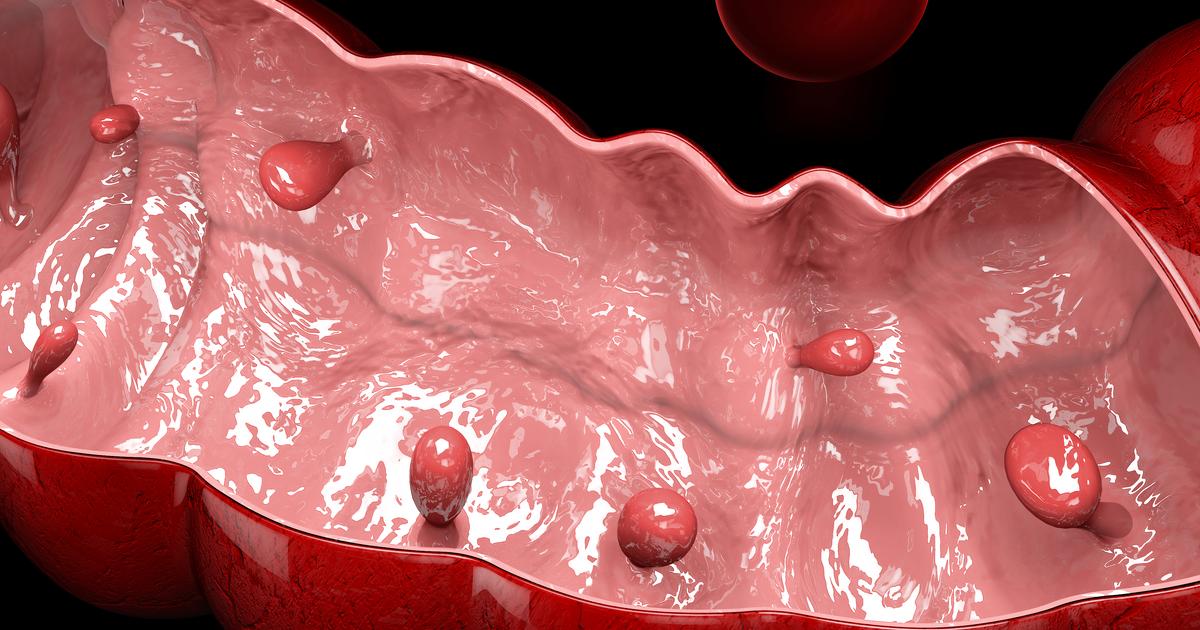
An individual affected by familial adenomatous polyposis may be at a higher risk of developing colon cancer than an individual who is not. Familial adenomatous polyposis is a genetic condition that causes an affected individual to develop hundreds of colon polyps. An adenomatous polyp is an abnormal growth or mass of healthy cells inside the intestinal tract. Familial adenomatous polyposis occurs in an individual when they have a mutation or alteration in the APC or MUTYH gene of their DNA that has been inherited from their parents.
The adenomatous polyps that grow inside of the intestinal tract should be treated with a surgical procedure to completely remove the polyps to decrease the risk of colon cancer development. Once familial adenomatous polyposis is diagnosed and adenomatous polyps are discovered in the intestines, yearly colonoscopy screening is recommended until a colectomy can be performed.
