Guide To Treating And Preventing Ventricular Fibrillation
Ventricular fibrillation is an irregular heart rhythm that occurs in the ventricles (lower chambers of the heart). This type of fibrillation is considered a medical emergency and requires immediate treatment. If left untreated, most cases of ventricular fibrillation will lead to cardiac arrest and death. Typically, loss of consciousness is the main symptom of this emergency. Before that, some patients may experience chest pain, rapid heart rate, dizziness, nausea, and shortness of breath. Patients with ventricular fibrillation will not have a pulse, and their electrocardiogram readings will be erratic or completely absent.
Individuals at an increased risk for ventricular fibrillation include those who have previously had a heart attack and individuals with congenital heart defects. Patients who have potassium or other electrolyte imbalances and individuals who have used cocaine or other illegal drugs are also at increased risk. Ventricular fibrillation can be caused by heart failure, cardiomyopathy, shock, long QT syndrome, electrocution, and Brugada syndrome.
Implantable Cardioverter-Defibrillator
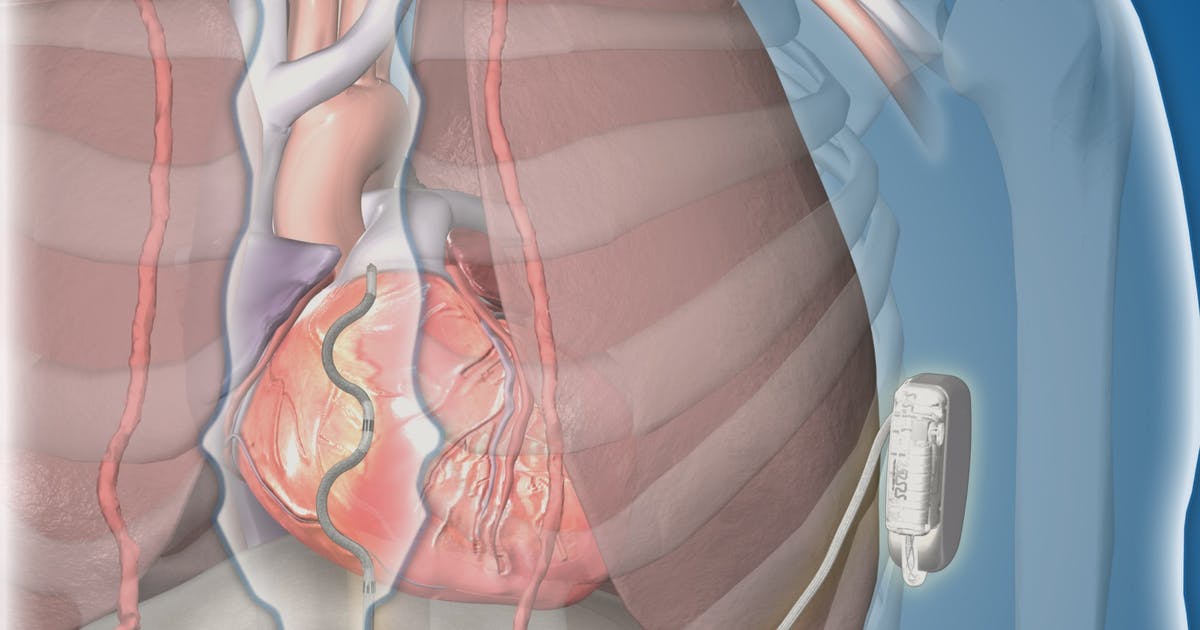
An implantable cardioverter-defibrillator (ICD) is a device that can prevent cardiac arrest and death in patients who have survived previous episodes of ventricular fibrillation. The device is also appropriate for patients who have a high risk of the condition and other types of abnormal heart rhythms. These devices are battery powered, and surgeons place them just underneath the skin, connecting them to the heart muscle through thin wires. They continuously monitor the patient's heart rhythm. If an abnormal rhythm is detected, they will deliver an electric shock to correct this and make the heart beat normally again.
Some implantable cardioverter-defibrillators also serve as pacemakers and can help speed up heart rhythms that are too slow. Patients who have ICDs need to be aware of their surroundings and avoid strong electromagnetic fields; these can prevent the ICD from functioning properly. Patients should also limit or avoid spending time around metal detectors, anti-theft devices, electric fences, and invisible pet fences. When using cell phones and headphones, patients should make sure these are used at least six inches away from their ICD. Cell phone chargers should be used at least twelve inches away from these devices.
Coronary Bypass Surgery

Coronary bypass surgery, which is performed under general anesthesia, can be used to reduce the risk of ventricular fibrillation by increasing blood flow to the heart. Surgeons bypass a damaged blood vessel in the heart, rerouting blood flow with a healthy blood vessel taken from another part of the patient's body. Both open surgery and newer, less invasive methods are available for this operation. Some cases may require open surgery. Following a bypass operation, patients are taken to the intensive care unit, and most stay there for two days. During the first day in intensive care, patients may be on a ventilator that breathes for them, and they may also have a stomach tube, a urinary catheter, an arterial line, chest tubes, and intravenous lines in place.
Most patients can have the majority of these tubes and lines removed on the second day, and they can also begin eating again. On the third day in the hospital, most patients are moved to a regular hospital ward and may stay there for a further two days. After discharge, recovery continues at home, and most patients will be fully recovered in six to eight weeks. Many patients choose to participate in a cardiac rehabilitation program during their recovery. In this program, patients participate in a supervised exercise program and are taught about healthy nutrition.
Anti-Arrhythmic Medication

In the emergency room, doctors treat ventricular fibrillation with several types of anti-arrhythmic medication. These medications include vasopressin and amiodarone, and are given to restore a normal heart rhythm after doctors have used an automatic defibrillator at least three times. For long-term prevention of additional episodes of ventricular fibrillation, doctors may recommend amiodarone for patients who cannot have an implantable cardioverter-defibrillator. Side effects of amiodarone include nausea, lack of coordination, tremors, fatigue, insomnia, and constipation.
For most patients who have survived ventricular fibrillation or are at high risk of an episode, doctors prescribe beta blockers, which reduce blood pressure and help improve blood flow. Examples of commonly prescribed beta blockers include atenolol, nebivolol, and propranolol. Beta blockers can cause changes in cholesterol levels, shortness of breath, fatigue, cold hands and feet, and weight gain. Depression and sleeping problems have also been reported.
Get Regular Exercise

Patients who have heart rhythm abnormalities and are at risk for ventricular fibrillation are advised to get regular exercise, as exercise helps strengthen the heart muscle and allows it to pump blood through the body more efficiently. Before beginning any exercise regimen, patients with heart conditions should have a physical examination to make sure they are healthy enough. In general, light exercises such as gentle yoga, slow swimming, tai chi, and walking are safe for cardiac patients.
Doctors generally recommend patients try to exercise 150 minutes per week. While exercising, patients should stop immediately if they experience any difficulty breathing or have chest pain, and a doctor should be informed. Instead of exercising on their own, patients may want to consider joining a group exercise class for individuals with health concerns or heart problems. These classes provide safe exercise methods and modifications so all patients can feel comfortable participating.
Consume A Healthy And Balanced Diet

Individuals at risk for ventricular fibrillation need to keep their blood pressure, cholesterol, and weight within safe limits. To help with this, doctors recommend patients consume a healthy and balanced diet. The DASH diet and the Mediterranean diet may both be beneficial for cardiac patients. These diets are based around fruits, vegetables, whole grains, legumes, nuts, fish, and limited amounts of oil. Patients recovering from heart surgery and those who have multiple health conditions may wish to consult a nutritionist, who can help with healthy meal planning. Patients should ask their doctors if there are any foods they should avoid that may interact with their medications. In particular, cardiac patients are advised to limit their intake of sodium and sugar.
