How To Treat Cystitis
We do not think about it a lot, but the bladder plays a very important role in keeping the body healthy. If something happens to the bladder, an individual can end up with a lot of pain and other unpleasant symptoms. Cystitis is characterized by bladder inflammation and typically occurs due to a urinary tract infection. Another cause is imbalanced bacteria in the urinary tract. When someone has this condition, they might experience urination changes and urges to urinate, back or abdominal cramping, urine that smells strongly or is cloudy, blood in the urine, and painful intercourse. When cystitis is acute, it tends to resolve by treating the underlying cause, such as a urinary tract infection. However, it can also become a chronic issue, referred to as interstitial cystitis, which affects up to twelve million individuals every year and tends to require more extensive care to avoid complications, such as a reduced bladder capacity and chronic pelvic pain.
Start reading now to get to know the most commonly used treatments for cystitis and its chronic counterpart now.
Bladder Distention

Bladder distention, where the doctor will fill the patient's bladder, might be considered to stretch the bladder. This procedure might help the bladder to handle more urine, giving patients have less urgency and frequency of urination. Bladder distention might be done more than once if patients get enough benefit, and in some cases, medicines such as dimethyl sulfoxide might be instilled into the bladder as part of this process. A catheter is used to get them into the bladder, and local anesthetic might be mixed in as well. For this procedure, the medication is instilled, stays in place for about fifteen minutes, and then patients are asked to urinate to expel it.
Keep reading to discover more treatments for cystitis.
Surgery

While doctors typically only recommend bladder surgery for patients who have severe pain and extremely diminished bladder function, three procedures might be considered if nothing else helps their symptoms. Surgical procedures might be helpful to improve a patient’s ability to control their bladder or to reduce severe pain. Fulguration is a minimally invasive procedure that works to burn off ulcers, which some patients with chronic cystitis develop in the bladder. It uses small incisions and instruments to access the bladder.
Resection is another minimally invasive choice, and it too works to remove any ulcers. The third surgical procedure is bladder augmentation, the purpose of which is to increase the bladder’s capacity to alleviate some of the urinary symptoms. The bladder receives a patch of the intestine to hold more volume. This does improve capacity, but it does not always reduce pain and may require patients to use a catheter to go to the bathroom.
Continue to unveil the next treatment option employed for cystitis.
Nerve Stimulation
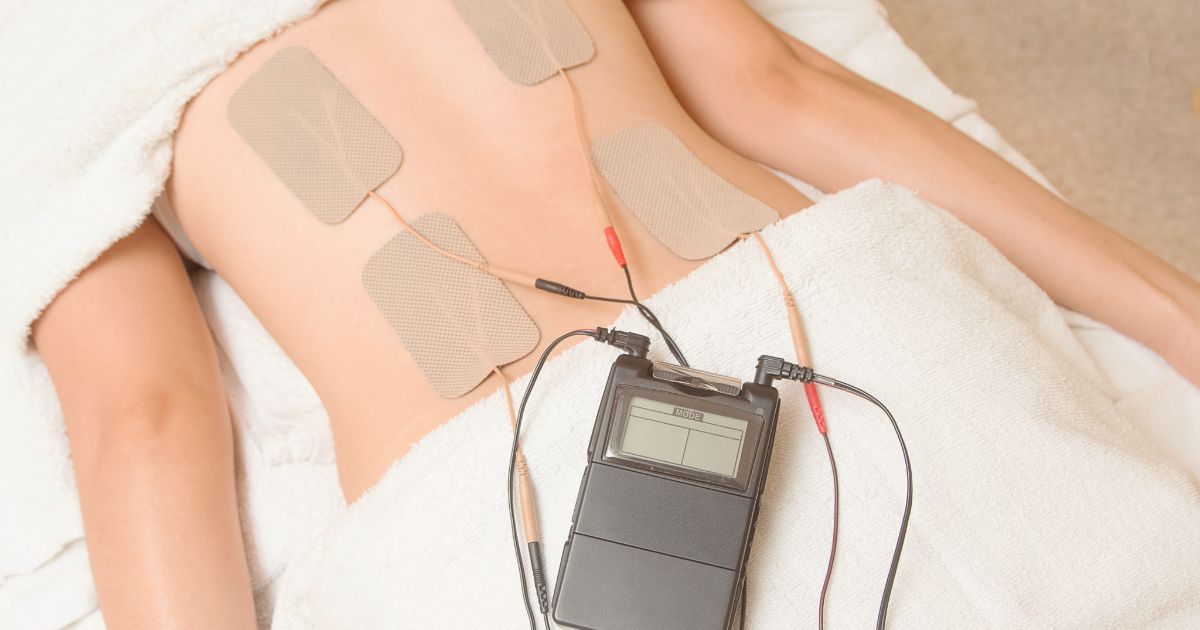
There are two nerve stimulation methods patients might benefit from. Transcutaneous electrical nerve stimulation (TENS) may help reduce urinary frequency and pelvic pain and works by sending mild electrical impulses to attempt to increase how much blood is flowing to the bladder. This might help to reduce pain by triggering certain substances that help to inhibit pain, and may also aid in bladder muscle strengthening to reduce urinary leakage. The low voltage electrical impulses are delivered with wires placed strategically on the pelvic and lower back areas. This electrical current keeps the body from being able to properly send painful sensations along the nerves to the brain. It can also help boost bladder flow to a region that can be used to speed up healing of the bladder.
Sacral nerve stimulation targets the sacral nerves, which are a crucial link between the bladder and the spinal cord. Helping stimulate them could result in decreased urinary urgency. In this procedure, the doctor puts a wire close to the sacral nerves. This type requires surgery for long-term device implantation where TENS does not. Sometimes a healthcare professional will show patients how to use these machines and adjust their settings so treatment can continue at the patient's home.
Keep going for information on more ways to treat cystitis.
Antihistamines

Antihistamines are a type of medication that dampens the body's immune system response. When patients take an antihistamine, their body quits responding to histamines, a chemical the body produces when it encounters an infection or harmful microorganism. This means they keep the immune system from kicking into overdrive and causing swelling, inflammation, increased blood flow, and more sensitive nerves. Though these drugs are most commonly used to treat allergic reactions, they can also be used as a method of managing interstitial cystitis. An antihistamine can help with this condition by reducing the inflammation that can cause pain and frequent urination. The most common antihistamine is hydroxyzine, though diphenhydramine and loratadine are also used occasionally because patients can get them over-the-counter. Antihistamines are generally a safe and effective method of managing interstitial cystitis, but they can cause extreme drowsiness in some patients.
Learn more about treating cystitis now.
Anti-Inflammatory Medication

Anti-inflammatory medication has roughly the same response as an antihistamine in that it keeps the body from producing inflammation in the bladder region, so patients are less likely to experience the swelling that causes discomfort and frequent urination. This medication keeps the body from producing prostaglandins, a type of chemical that results in higher levels of inflammation. This can cut back on the inflammation that may cause so much damage to the bladder. A nice side effect of taking anti-inflammatories is that many of these types of medication are also painkillers, which means they can help manage the painful symptoms of interstitial cystitis while simultaneously addressing the root of the issue. Common medications that doctors prescribe for patients who want anti-inflammatories include acetylsalicylic acid, ibuprofen, and naproxen sodium. However, keep in mind these typically are not advised for constant, long term usage. Instead, they are most effective when taken occasionally to address particularly unpleasant pain or heightened inflammation.
Uncover details on more treatment methods now.
Physical Therapy

Not all forms of pelvic pain are strictly due to the bladder itself. All the swelling and inflammation in the area can also affect a variety of pelvic muscles. This can further worsen the problem by causing overly tense or sore muscles that do not properly aid the body in urinating, having sex, and moving around. Some patients also have various muscle abnormalities and connective tissues issues that can directly cause cystitis and eventually interstitial to develop. For patients with any of these issues, physical therapy is a good solution. A physical therapist can address all sorts of muscle problems that are either causing or caused by this condition. This type of treatment usually involves the therapist assessing the patient and identifying any potential causes of problems. Then they guide the patient through stretches and exercises that can help strengthen and loosen the muscles until the patient's body is properly aligned.
Get to know another treatment option for cystitis now.
Antibiotics

Antibiotics are commonly used for cystitis in a course spanning three to ten days. Symptoms usually begin to alleviate within the first day or two of using antibiotics. The most common antibiotics recommended for cystitis include trimethoprim-sulfamethoxazole, cephalosporins, levofloxacin, nitrofurantoin, amoxicillin, and ciprofloxacin. It is important to start the antibiotics promptly and take the full course. This is especially important for women who are pregnant and those with other medical conditions that weaken their immune systems. Following the full course, if a patient is still having symptoms, they should talk to their doctor because further treatment might be necessary.
