What Are The Most Common Lung Diseases?
Lung disease describes any issue that occurs in the lungs that inhibits them from functioning as they should. The lungs are an element of an intricate mechanism that relaxes and expands thousands of times a day to perform the oxygen and carbon dioxide exchange. Oxygen is essential for the cells throughout the body to operate properly. Lung diseases are the result of issues that occur within this mechanism.
There are three different subclasses of lung diseases. Lung tissue diseases are those that alter or have adverse effects on the structure of the lung. Airway diseases have adverse effects on the tubes that carry oxygen in and carbon dioxide out of the lungs. Lung circulation diseases negatively affect blood vessels that run throughout the lungs. Some lung diseases may fall into more than one of these three subclasses.
Asthma

One of the most prevalent lung diseases that cause problems in airways is asthma, a condition where the airways inside of an individual's lungs become narrowed and swollen. Depending on the type of asthma an individual is affected by, extra mucus may also be produced by the lungs. The severity of asthma varies from one individual to the next. Symptoms of asthma include wheezing, coughing, difficulty breathing, and breathlessness. Asthma can be induced by an individual's allergies or physical activity. Certain irritants present in some workplaces can trigger symptoms in an individual affected by occupational asthma.
A physical examination, lung function tests, methacholine challenge, nitric oxide test, and diagnostic imaging tests may be used to diagnose an individual with asthma. Treatment includes daily long-acting medications to keep the airways open, avoidance of potential triggers, short-term medications to open the airways, and allergy medications.
Pneumonia

Pneumonia is a lung disease that affects the alveoli or air sacs in the lungs. Numerous germs can cause an individual to develop pneumonia, including bacteria, fungi, and viruses that come in contact with the lungs. Even small pieces of aspirated food can cause someone to develop pneumonia. The air sacs or alveoli in a patient with pneumonia tend to fill up with purulent material or pus. Symptoms include a cough that produces phlegm or pus, difficulty breathing, chills, chest pain when breathing and coughing, confusion, fatigue, nausea, vomiting, shortness of breath, and fever.
A patient's pneumonia is diagnosed with the use of blood tests, pulse oximetry, sputum test, chest x-ray, CT scan, and pleural fluid culture. An individual affected by pneumonia may be treated with antibiotics if their infection has been caused by bacteria. Medications used to dislodge sputum and suppress a patient's cough may be part of their pneumonia treatment. Pain relievers and fever-reducing medications are used to ease pain and discomfort associated with a fever and pneumonia.
Pneumothorax
A lung disease that causes a dangerous structural alteration and impairment of function is referred to as pneumothorax, which refers to a lung that has collapsed. A lung can collapse due to several different mechanisms. At some point, an opportunity is provided for air to enter the space in between an individual's chest wall and lung. The air in this space creates pressure placed directly on the individual's lung, causing it to collapse. This process usually occurs as a result of a blunt chest injury, damage from underlying lung disease, and certain medical procedures. Symptoms that occur upon the collapse of a lung include shortness of breath and sudden chest pain. An individual who has had a pneumothorax before is more likely to experience another within two years following the first.
Diagnosis of pneumothorax is typically made through the use of computerized tomography scans, ultrasound imaging, and chest x-rays. Treatment focuses on releasing the pressure inside of the patient's chest cavity to allow the lung to re-inflate properly. A needle aspiration, chest tube insertion, surgery, or nonsurgical repair may be used to accomplish this goal.
Bronchitis

When an individual's larger lung airways become inflamed, it is referred to as bronchitis. The passages through which air passes through from an individual's mouth and nose to their lungs are referred to as bronchi. Bronchitis occurs when an infection or another mechanism causes the lining of the bronchi to become irritated and inflamed. Bacteria, viruses, and other types of particles that irritate an individual's bronchi can cause bronchitis. This inflammation makes it difficult for an affected individual to inhale air and effectively breathe oxygen into their lungs. In addition, inflammation of the bronchi lining impairs the patient's ability to clear phlegm and heavy mucus from their airways. Symptoms of bronchitis include persistent mucus-producing cough, low-grade fever, chest tightness, body aches, headaches, wheezing, chills, sore throat, blocked nose, breathlessness, and obstructed sinuses. Bronchitis is diagnosed with the use of x-rays, blood tests, and lung function tests. This condition is treated with cough medications, oxygen therapy, anti-inflammatory drugs, bronchodilators, and mucolytics.
Chronic Obstructive Pulmonary Disease

Chronic obstructive pulmonary disease (COPD) is a disease that causes damage to the bronchi or larger branches in the lung that carry air to smaller branches. COPD is an umbrella term used to encompass two different long-term diseases that occur concurrently, including the chronic form of bronchitis and emphysema. The combination of these lung diseases causes the airways to swell severely and results in an impaired ability to breathe in and out. Symptoms of chronic obstructive pulmonary disease include shortness of breath, wheezing, chest pain, persistent cough, and chest tightness. COPD that has progressed to a severe stage can result in symptoms such as appetite loss, sexual dysfunction, blue lips, fatigue, morning headaches, depression, sleep problems, blue nail beds, frequent infections of the lungs, and weight loss. Diagnosis of this condition is made using a physical examination, pulse oximetry, pulmonary function tests, computerized tomography scans, chest x-rays, and blood tests. Treatment for COPD includes the administration of bronchodilators, steroid medications, mucolytics, oxygen therapy, protein therapy, administration of vaccines, and surgery.
Pulmonary Edema

Pulmonary edema is a lung condition where excess fluid accumulates in the air sacs or alveoli, causing problems with the function and structure of the organs. Pulmonary edema can be caused by problems with heart structure or function, or it can be caused by nervous system conditions, high altitudes, acute respiratory distress syndrome, adverse drug reaction, pulmonary embolism, smoke inhalation, near drowning, infections, and toxin exposure. Symptoms of pulmonary edema include breathlessness, wheezing, clammy skin, blue-tinted lips, palpitations, rapid weight gain, lower extremity swelling, fatigue, anxiety, productive cough, fever, chest discomfort, headaches, difficulty with exercise, and shortness of breath upon exertion or lying down. Pulmonary edema is diagnosed with the use of a physical examination, pulse oximetry, blood tests, echocardiogram, chest x-rays, cardiac catheterization, and electrocardiogram. Treatment for pulmonary edema may include administration of supplemental oxygen, diuretic medications, morphine, blood pressure medications, and in rare cases, therapy in a hyperbaric chamber.
Pulmonary Embolism
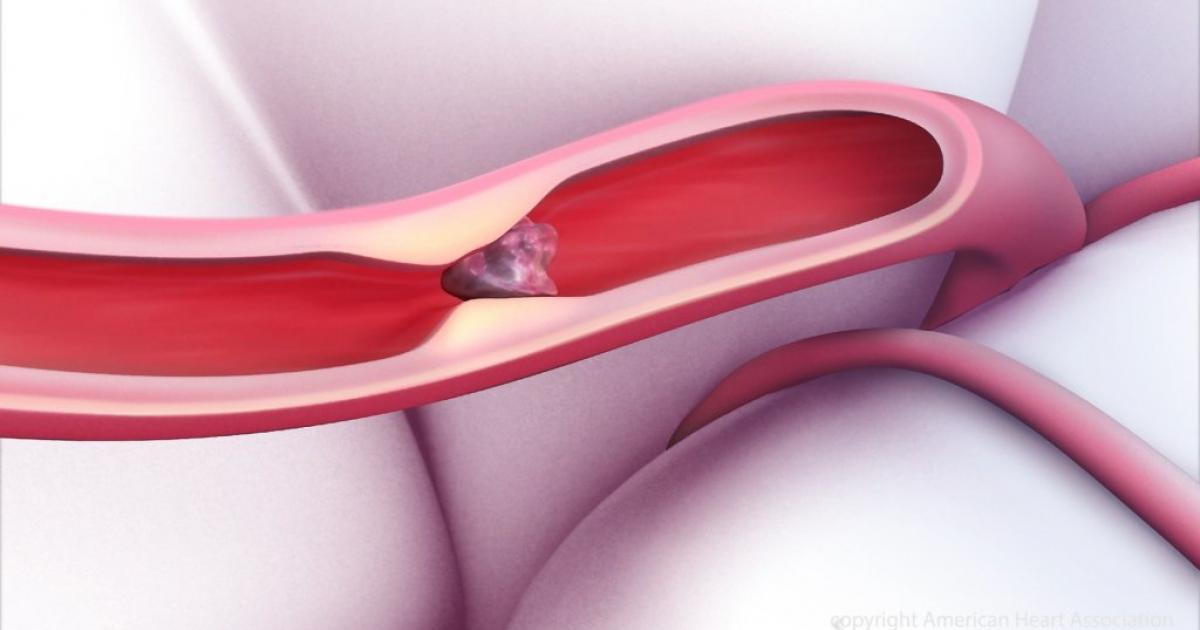
Pulmonary embolism is a life-threatening condition where a blood clot becomes lodged in the lung tissues. A blood clot in the lung tissues can cause tissue damage as a result of the deprivation of blood. Pulmonary embolism can cause oxygen levels in the patient's blood to become too low, which can cause damage to other vital organs in the body from the insufficient oxygen supply. Symptoms of pulmonary embolism include shortness of breath, productive or unproductive cough, chest pain, back pain, more sweating than usual, lightheadedness, syncope, and blue tint in the lips or nails. A diagnosis of pulmonary embolism is made through physical examination, ultrasound of the lungs, x-rays of the lungs, blood tests, computed tomographic angiography, ventilation/perfusion scan, pulmonary angiography, MRI scans, and echocardiogram. Treatment includes the short or long term administration of anticoagulants to help prevent the body from forming new blood clots inappropriately, such as warfarin, heparin, dalteparin, enoxaparin, and tinzaparin.
Lung Cancer
The lungs are the two delicate organs in the chest cavity that facilitate the exchange of oxygen and carbon dioxide in the blood before it is pumped by the heart back to the tissues in the rest of the body. Lung cancer is a common lung disease, leading the United States in most deaths attributed to cancer. Most cases of lung cancer are caused by smoking cigarettes and exposure to other carcinogens commonly found in certain occupations. A small percentage of lung cancer cases occur in individuals who do not smoke because of genetic factors and a general predisposition to developing cancer. Symptoms of lung cancer include a productive cough that will not go away, hoarseness, unintentional weight loss, headaches, bone pain, chest pain, shortness of breath, and coughing up blood in small or large amounts. A diagnosis of lung cancer is made with the use of sputum cytology, x-ray imaging, CT scans, and lung tissue biopsy. Treatment options include surgery, radiosurgery, chemotherapy, radiation therapy, immunotherapy, and palliative care.
Emphysema

Emphysema is a lung condition where the small air sacs (alveoli) in the lungs incur damage and do not function properly. As the condition progresses, the alveoli become weakened and eventually burst. The surface area of the inside of the lungs becomes decreased, and symptoms occur because there is no room for new oxygenated air to enter. Symptoms of this condition include slow but progressive shortness of breath. At first, it only occurs upon exertion but eventually progresses to shortness of breath even while at rest. Emphysema patients experience shortness of breath to the point where they are unable to climb stairs, their lips and fingernails become pale or discolored upon exertion, and they experience changes in their ability to stay mentally alert upon exertion. An emphysema diagnosis is made with the use of chest x-rays, CT scans, blood testing, physical examination, and lung function tests. Treatment for this condition often includes inhaled steroid medications, antibiotics, bronchodilators, nutrition therapy, pulmonary rehabilitation, supplemental oxygen, lung volume reduction surgery, and lung transplantation.
Pleural Effusion

Pleural effusion is a condition where the space between an individual's chest cavity wall and the lungs, the pleural space, becomes filled with more fluid than normal. An individual's lung and chest cavity are lined with pleura or special membranes that contain a small amount of fluid that is meant to keep them moist and reduce friction. There are many possible causes of pleural effusion, including kidney or liver disease, autoimmune disorders, pulmonary embolism, cancer, congestive heart failure, certain respiratory infections, and complications from specific medical procedures. A pleural effusion patient may have symptoms such as unproductive cough, chest pain, shortness of breath, inability to take deep breaths, problems with breathing when lying down, fever, and painful breathing. An individual who has common bouts of hiccups that are difficult to diffuse may also have pleural effusion. A diagnosis of pleural effusion is made with a physical examination, x-ray, CT scans, kidney function tests, liver function tests, lung biopsy, bronchoscopy, and echocardiogram. Treatment for this condition may include chest draining, pleurodesis, and surgery.
