Symptoms Of Pancreatitis To Look Out For
Pancreatitis is a medical condition that causes the pancreas to become inflamed. Pancreatitis can develop due to gallstones, cystic fibrosis, infections, pancreatic cancer, and abdominal surgery. Elevated calcium and triglycerides are also risk factors for this condition. If left untreated, pancreatitis may lead to breathing difficulties, malnutrition, and kidney failure.
There are many options for pancreatitis treatment. Patients may need to engage in fasting for a few days, especially with a hospital visit. Pain medications also help treat pancreatitis, though many patients require intravenous fluids to stop dehydration with pancreatitis. Surgery for pancreatitis may also be necessary. For instance, patients may need a gallbladder removal. A pancreatitis cure often means dietary changes and pancreatic enzyme supplements.
Poor Absorption Of Food

The poor absorption of food, also known as malabsorption, typically occurs in chronic pancreatitis. With chronic pancreatitis, the normal function of the pancreas may be significantly impaired. Thus, it will not release a sufficient number of the enzymes required to break down food effectively. This can lead to both diarrhea and significant weight loss. Stools may also be lighter in color than normal. A stool test can be used as part of a diagnostic workup to identify malabsorption; it may show excessive fat in the stool. To treat the poor absorption of food, doctors will monitor patients for dehydration. They will likely be referred to a nutritionist for consultations. Dietary changes can help patients obtain more nutrients, and patients may need to take vitamin and enzyme supplements.
Keep reading for more information regarding the symptoms of pancreatitis now.
Swelling And Tenderness In The Abdomen

Both acute and chronic pancreatitis produce swelling and tenderness in the abdomen. Abdominal tenderness is more common in acute pancreatitis, and this typically occurs when the abdomen is touched. Patients with acute pancreatitis generally experience tenderness accompanied by pain in the upper abdominal area. The pain may radiate to the patient's back, and it usually worsens after a meal. Abdominal tenderness is less common in chronic pancreatitis, but patients frequently experience upper abdominal pain. In chronic cases, this pain may be more constant, and it may not come and go with meals.
Most patients with any kind of pancreatitis will have severe abdominal pain, and hospitalization is often required. To reduce swelling and pain, patients may fast for several days during their hospital stay and then transition to a liquid diet for a short time. Once food is reintroduced, patients may need to follow a low-fat diet. Nutritionists can help them create meal plans that ease pain associated with eating and digestion. The use of a feeding tube may be needed for patients whose pain persists after eating. Both oral and intravenous pain medications will also be given to ease pain. Patients may be able to take enzyme supplements to improve their digestion.
Learn more about the warning signs of pancreatitis now.
Diabetes

Diabetes is a possible complication that may occur due to chronic pancreatitis, which causes pancreatic scarring and damage. It is a condition in which the body cannot use insulin effectively, resulting in persistently elevated glucose in the blood. Possible signs of diabetes include excessive thirst, frequent urination, blurry vision, fatigue, bruises or cuts that are slow to heal, and weight loss. Patients may also deal with tingling sensations in the hands or feet. They may also feel numb.
Patients will need to monitor their blood glucose levels according to the schedule set by their physician. Dietary alterations and an exercise regimen may help patients reduce their glucose. If these are not enough, patients may be prescribed oral medication to improve their glucose control. Some injectable medication may also be used. These medications may be combined with insulin injections. Patients with diabetes are typically treated in the long-term by an endocrinologist.
Get the details on more pancreatitis symptoms now.
Upper Abdominal Pain

Pain in the upper abdominal quadrant is one of the most common and distressing symptoms of chronic and acute pancreatitis. The pancreas is located in the upper abdomen just behind the stomach. Thus, pain from pancreatitis usually begins in the upper abdominal area. In acute pancreatitis, the pain may occur with nausea and vomiting. Oily stools (steatorrhea) typically accompany chronic pancreatitis. Since upper abdominal pain from this condition is generally severe, patients may be referred to a pain management specialist for advanced care. Avoiding dietary fat may provide some relief, and narcotic pain relievers may be indicated.
Depending on the cause of pancreatitis, some patients may gain pain relief through surgical procedures. For example, if pancreatitis is caused by gallstones, removing the gallbladder can alleviate pain. Patients whose pancreatitis is the result of a bile duct obstruction may be able to have a procedure to correct this. In some cases, draining fluid from the pancreas and removing diseased pancreatic tissue may provide a degree of pain relief.
Discover more pancreatitis symptoms now.
Increased Heart Rate

An increased heart rate is typically associated with acute pancreatitis. It may occur together with a fever. Doctors define an elevated heart rate as any rate above one hundred beats per minute. To check the patient's heart rate, a doctor or nurse will measure the patient's pulse at the wrist. Patients in the hospital undergoing treatment for pancreatitis will have their pulse and blood pressure checked every few hours. An ECG monitor will provide doctors with continuous monitoring of the patient's heart rate and rhythm. Patients who notice their heart rate is increasing or feel any skipped beats or pain in their chest should alert their doctor or nurse. While the heart rate will typically return to normal once pancreatitis is resolved, medications to slow down the rate can be given.
Uncover more symptoms linked to pancreatitis now.
Fever

A fever is an abnormal total increase in an individual's body temperature. Pancreatitis patients may experience a fever because the tissues in the pancreas have become inflamed and infected. When tissues in the body become inflamed or damaged, the immune system responds to mediate that damage. One component of this immune system response is increasing the thermostat of the individual's body to make it an inhospitable environment for pathogens that could cause tissue inflammation or damage. The immune system sends signals to the hypothalamus, telling it to raise the total body temperature above normal. While a fever may seem beneficial in many situations where pathogens are causing tissue damage, it can also damage healthy tissues around the body when the temperature becomes too high.
Continue reading to learn more about the potential warning signs of pancreatitis now.
Nausea And Vomiting

Nausea occurs when an individual feels like they need to vomit. Vomiting describes the forceful actuation of contents from the stomach up through the esophagus and out of the mouth. Nausea is a sensation activated in an individual's brain when the body experiences an abnormal buildup of toxic substances, or when digestive organs and structures become inflamed. A pancreatitis patient may experience nausea and vomiting because of an obstruction in the duct that carries pancreatic enzymes and bile to the small intestine. A blockage in this duct causes the accumulation of bilirubin in the blood, which can activate the brain's nausea center. Additionally, the nerve fibers of the nerves surrounding the pancreatic tissue that has become swollen, inflamed, and infected can become irritated and activate the nausea center in the brain.
Reveal additional pancreatitis symptoms now.
Steatorrhea

Steatorrhea is a term used to characterize when an individual's stools have too much fat content. An individual affected by steatorrhea has stools that are foul-smelling, unusually bulky, and pale. Steatorrhea tends to float and may be covered in a greasy-like film due to the higher fat and gas content. The presence of steatorrhea means an individual's digestive system cannot digest and absorb certain nutrients such as dietary fats the way it should. Certain digestive enzymes and other substances are required to help break down the nutrients in food when they reach the stomach and small intestine. When specific enzymes or digestive substances are not secreted into the stomach or small intestine to assist with digestion, the non-digested nutrients will remain in the stool until it is excreted. When the pancreas is inflamed or infected due to pancreatitis, it cannot secrete digestive enzymes required for the digestion of dietary fats. When these fats remain in the stool when it is excreted, it causes steatorrhea.
Discover additional severe symptoms of pancreatitis now.
Jaundice
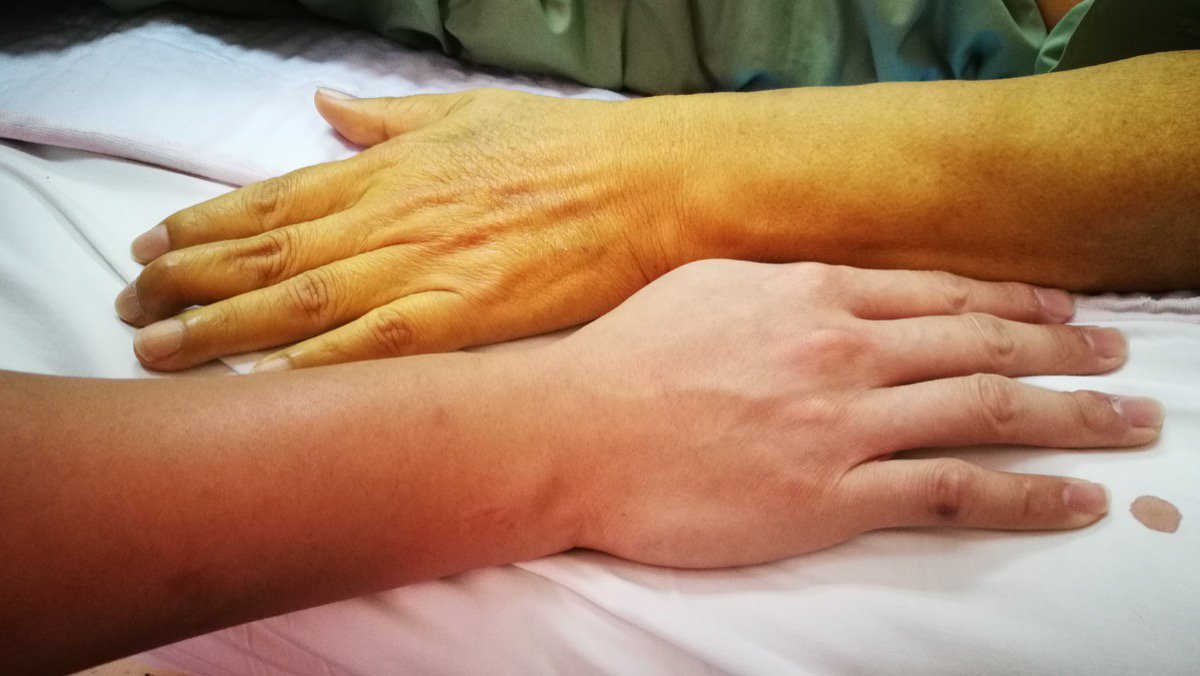
Jaundice describes when an individual develops a yellow tint to their skin or whites of their eyes due to an accumulation of bilirubin in their body. The hemoglobin molecules inside of red blood cells that have died are recycled inside the liver and are synthesized into bilirubin. Bilirubin is then concentrated inside the gallbladder to produce bile, a substance required for the intestines to digest fatty foods properly. A pancreatitis patient may have developed this infection because they have an obstruction in the ducts that carry both digestive enzymes from the pancreas and bile from the gallbladder into the small intestine. When bile is prevented from draining into the small intestine, it builds up in the blood and other organs. Bile and bilirubin are both substances with a potent yellow pigmentation, which causes jaundice.
Get more details on the warning signs linked to pancreatitis now.
Diarrhea

Diarrhea is when stool is looser and more watery than usual. Diarrhea occurs when the food individuals consume moves too rapidly through their large intestine and is excreted. The large intestine or colon absorbs fluid from the foods consumed and digested by the stomach and small intestine before it is eliminated from the body. When food does not stay in the large intestine long enough, it causes diarrhea.
A pancreatitis patient can develop irritation in the nerves that neighbor the pancreas, which can stimulate the excessive contraction of muscles that play a significant role in digestive processes. When the muscles that work with the digestive organs to move food through the system contract excessively, food moves through the intestines too quickly. The large intestine is unable to absorb fluids from the intestinal content properly, and the patient experiences diarrhea.
