Guide To The Prevention And Treatment Of Diabetic Hyperosmolar Syndrome
Diabetic hyperosmolar syndrome develops as a result of extremely elevated blood glucose (normally at least six hundred mg/dL), and symptoms intensify over a few days or weeks. Patients with diabetic hyperosmolar syndrome may have a fever, and their skin is often warm and dry. Excessive thirst, drowsiness, confusion, and increased urine output are all common symptoms. Some patients may experience vision loss, hallucinations, or seizures.
This condition is considered a medical emergency that requires treatment at a hospital. If left untreated, patients may develop severe dehydration or fall into a coma, both of which may be life-threatening. Patients who have type 2 diabetes and are over sixty-five years old face an increased risk of this condition, as do individuals with kidney disease and heart failure. As a preventative method, doctors advise diabetes patients to seek immediate medical treatment if their blood glucose readings are higher than four hundred mg/dL. To diagnose diabetic hyperosmolar syndrome, doctors at the hospital will perform blood tests to check the patient's glucose levels.
The steps outlined below are routinely recommended for the prevention and treatment of diabetic hyperosmolar syndrome.
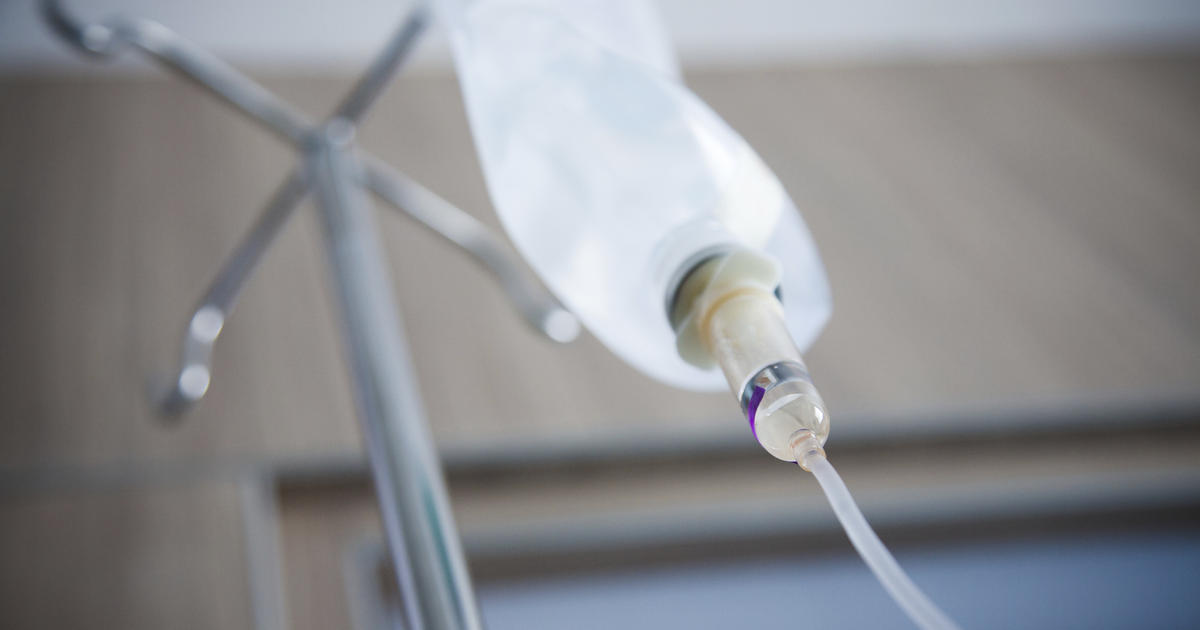
Intravenous Fluids for Dehydration

Intravenous fluids for dehydration are administered at the hospital for patients with diabetic hyperosmolar syndrome. While patients may sometimes be treated with oral rehydration, intravenous fluids are the most efficient and rapid treatment method, and they are especially crucial when the patient is severely dehydrated. Intravenous fluids are necessary for patients who have a weak pulse or rapid heartbeat and for those who are lethargic or unconscious. Fluids are given to replace both lost water volume and depleted electrolytes. Typically, medical staff will begin by administering Ringer's lactate solution (Hartmann's solution) or a normal saline solution. The amount of fluid administered is based on the degree of dehydration and the patient's weight. Severely dehydrated patients normally lose about ten percent of their normal fluid volume and need ten milliliters of fluids per each kilogram of body weight.
Uncover more information on the ways to prevent and treat diabetic hyperosmolar syndrome now.
Intravenous Insulin To Control Blood Sugar
Patients with diabetic hyperosmolar syndrome are routinely given intravenous insulin to control blood sugar as part of their emergency care. Regular insulin is the only form of insulin administered intravenously, and it begins to work within fifteen to thirty minutes. To give insulin intravenously, medical staff always use an infusion pump, and a separate insulin-only intravenous line is used. An insulin infusion is normally continued for at least thirty to sixty minutes, and patients will have their blood glucose checked approximately one hour prior to stopping the infusion. After the healthcare team has discontinued the intravenous insulin, the patient will have their blood glucose measured again at meals and before bedtime. Throughout the infusion process, doctors will monitor the patient's vital signs, and patients should report any new or worsening symptoms to staff.
Learn more about preventing and treating diabetic hyperosmolar syndrome now.
Replacement Of Potassium

Patients with this condition frequently experience a depletion in their levels of potassium, one of the key electrolytes in the body. Not enough potassium can cause weakness, and it places patients with diabetic hyperosmolar syndrome at an increased risk of developing serious heart rhythm abnormalities. While receiving intravenous insulin and fluids, patients will also receive an intravenous replacement of potassium. This will begin once doctors have established that the patient has a urine output. During the treatment, patients will have repeated blood tests to check their potassium levels, and the intravenous potassium will be stopped once doctors determine the patient's potassium levels have reached the normal range. Occasionally, patients receiving replacement potassium may also need to receive doses of intravenous sodium phosphate to ensure proper electrolyte balance. Since potassium levels can affect the heart, patients receiving potassium infusions will have their heart rate and rhythm monitored continuously with an electrocardiogram. In addition, doctors may periodically listen to the patient's heart with a stethoscope to check for any abnormal sounds, and patients should report any chest pain or dizziness to staff immediately.
Continue reading to learn more about how to prevent and treat diabetic hyperosmolar syndrome now.
Treatment For Underlying Conditions

Having an underlying condition is a strong risk factor associated with the development of diabetic hyperosmolar syndrome. Congestive heart failure and kidney failure are two of the most common underlying conditions patients with this syndrome may have. To promote a successful outcome, treatment for underlying conditions is normally provided at the same time as fluids and other treatments for diabetic hyperosmolar syndrome. Since patients may not be aware they have an underlying condition, they will be given a physical exam and blood tests at the hospital. Along with blood pressure screening and electrocardiogram monitoring, these checks can detect numerous underlying ailments. Occasionally, treatment for underlying conditions may require additional tests or procedures that need to be completed at a later date. In this case, hospital staff will focus on stabilizing the patient and getting their blood glucose back down to a normal range. Once the patient is stable and awake, additional investigations or medications for underlying conditions can be provided.
Get the detail on more options for preventing and treating diabetic hyperosmolar syndrome now.
Appropriate Diabetes Management Techniques

To prevent diabetic hyperosmolar syndrome, doctors advise all diabetes patients to follow appropriate diabetes management techniques. Patients should check their blood glucose readings as often as their doctor suggests, especially after meals and before bedtime. Keeping a log of blood glucose readings can help patients know when their readings are getting out of control, and these logs should be shared with the patient's healthcare team. In addition, patients should take all medications they have been prescribed. If a patient has questions about the dosage or administration method of a particular medicine, they should speak with the prescribing doctor to get more information. Patients should always report any medication side effects or unusual symptoms to their healthcare team. To keep their blood sugar under control, patients are also encouraged to be mindful of their nutrition and fitness. Specialist nutritionists can help patients devise meal plans that provide better blood sugar control.
