Ways In Which Stargardt Disease Is Diagnosed
Stargardt disease is a progressive eye condition that leads to macular degeneration, hampering the part of the retina responsible for clear central vision. Also known as juvenile macular degeneration and fundus flavimaculatus, the condition is inherited and has been linked to mutations of the ABCA4 gene. Stargardt disease typically results in significant vision loss during childhood or adolescence. While the majority of patients do not become completely blind, it is common for patients to have visual acuity of 20/200 or worse. The prevalence of Stargardt disease is estimated to be approximately one in every eight to ten thousand individuals.
In the early stages of this condition, patients generally notice gray, black, or blurry areas within their central visual field, and they may also find it takes their eyes longer than usual to adjust when moving from a sunlit room into a darker environment. Bright light may begin to irritate the eyes, and some patients lose color vision and some peripheral vision as the disease advances.
While there is currently no treatment for Stargardt disease, eye specialists frequently recommend for patients to avoid taking vitamin A supplements, which may accelerate vision loss associated with this disease, and both smoking and exposure to secondhand smoke should be avoided. Low-vision aids may make daily activities easier, and patients might benefit from occupational therapy and counseling services.
To diagnose Stargardt disease, eye doctors may perform the tests described below.
Optical Coherence Tomography
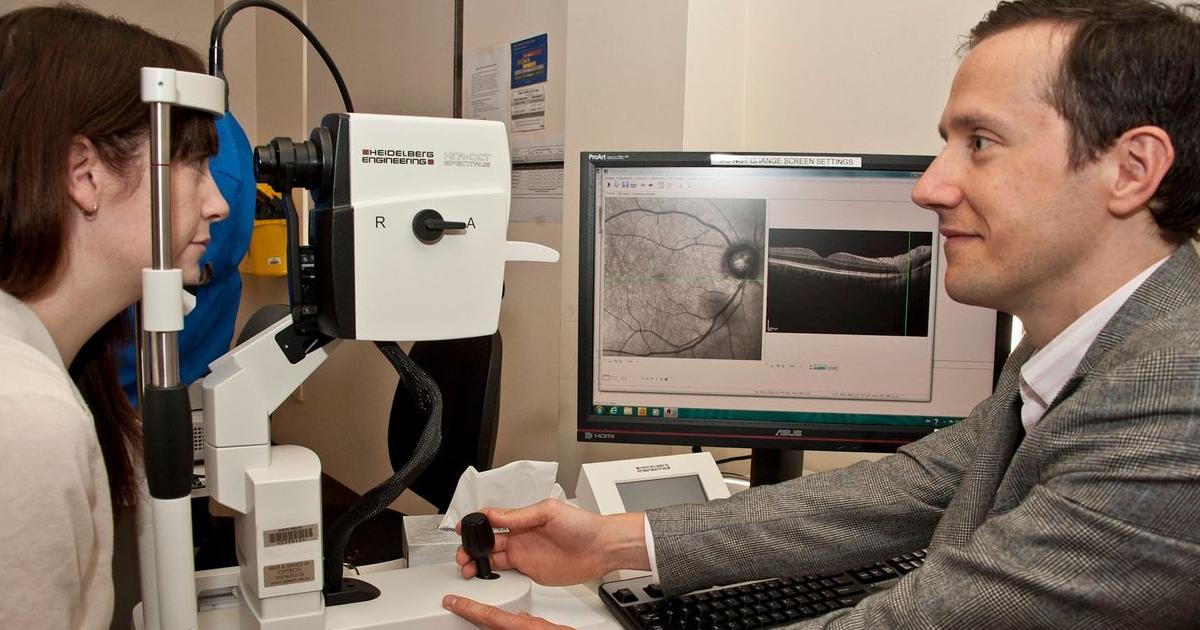
Optical coherence tomography is a noninvasive, painless test ophthalmologists perform to get a detailed view of each layer of the patient's retina. The test uses light waves to produce photos of cross-sections of the retina. This information enables the clinician to map the patient's retina and measure the thickness of each layer. Before having optical coherence tomography, the patient will need to have their eyes dilated. After administering a numbing drop, the ophthalmologist will place several dilating eye drops into each of the patient's eyes. Dilating the eyes widens the pupil, and this makes it easier for the doctor to perform a close examination of the retina.
Once the eye drops are working, the patient will sit in front of a special machine, resting their head on the machine to prevent movement. Next, the machine will scan both of the patient's eyes. This takes between five to ten minutes, and the machine will not touch the eyes during the scanning process. If dilating eye drops have been used, the patient may experience sensitivity to light for several hours, and it may be necessary for someone else to drive the patient home.
Uncover the next Stargardt disease diagnostic test now.
Visual Field Testing

The visual field is the width of the area a patient sees while focusing on a central point. A visual field test provides a measurement of how much vision the patient has in each eye, and it can also indicate the severity of any vision loss the patient might be experiencing. Visual field testing will alert clinicians to the presence and location of blind spots in the patient's central vision. To perform visual field testing, specialists typically start with the confrontation visual field test. While the patient looks at an object in front of them, one of their eyes will be covered. The doctor will show the patient different numbers of fingers within their peripheral vision, and the patient will be asked how many fingers were displayed.
For a more detailed screening, the clinician will perform an automated perimetry test. This procedure tests one eye at a time, and the patient will have the other eye covered with a patch. While the patient looks at a central target on a screen, lights will be shown on the screen in various areas of the visual field. The patient presses a button each time they see a light, and the machine records which lights the patient could and could not see.
Get the details on the next test used to diagnose Stargardt disease now.
Electroretinography

Electroretinography is a method of measuring the electrical response of the eye's rods and cones, specialized cells in the retina that sense light. The test takes roughly sixty minutes to complete. Before beginning the test, the doctor will administer numbing drops into each eye to prevent discomfort. Next, a speculum is placed on each eye to gently hold it open, and an electrode is placed on the corneas. The patient looks at a screen that displays both flashing lights and varied light patterns, and the electrode records how their retina responds to the lights. These readings are transmitted to a separate screen for viewing and recording. The test is first performed in a room with normal lighting.
After it is completed, the healthcare provider will dim the lights and give the patient twenty minutes of resting time for their eyes to adjust. After this period, the test will be repeated in the darkened room. Patients who have had this test performed should avoid rubbing their eyes for at least one hour after the procedure; doing so may scratch the corneas.
Learn more about how Stargardt disease is diagnosed now.
Color Testing
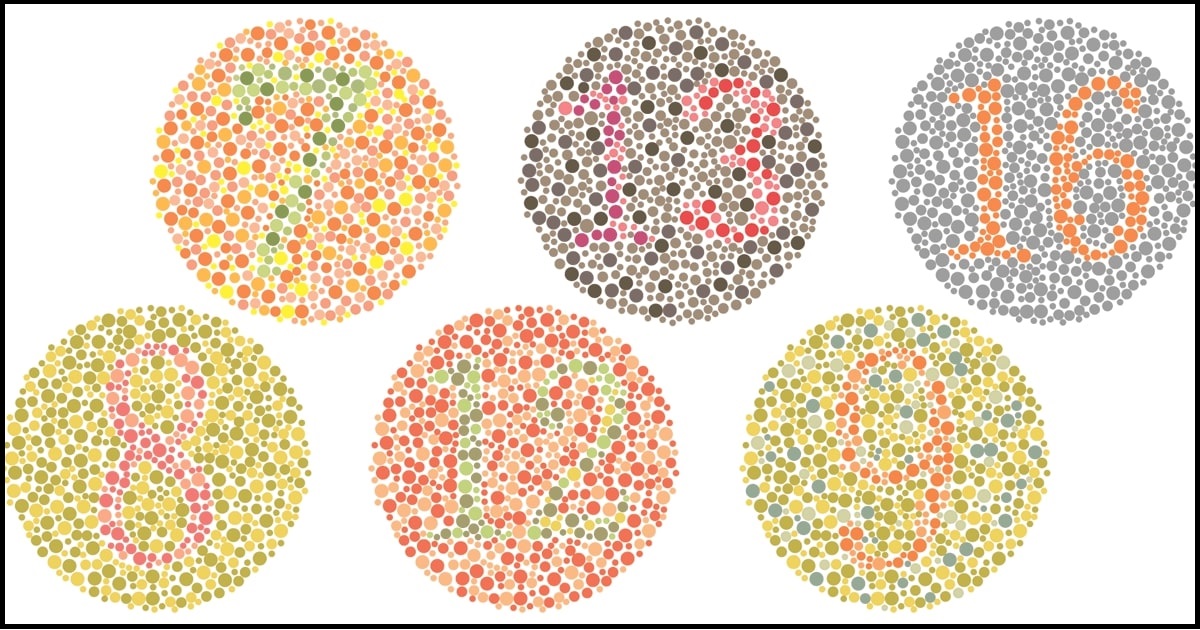
Color testing is especially useful for patients who may be experiencing the changes to their color vision that frequently occur in the later stages of Stargardt disease. The testing can also be beneficial as a screening tool. Plate tests are widely used to test color vision, and they involve the patient identifying a colored symbol embedded in a background. Other forms of plate testing ask the patient to choose which color in a series of four colors is most similar to a specific color, and patients could also be asked to determine which circle most closely matches the shade of a gray rectangle. Arrangement tests and lantern tests may be used in conjunction with plate testing, and some healthcare providers may opt to administer testing with the use of anomaloscopes.
Uncover more tests used to help diagnose Stargardt disease now.
Fundus Photo
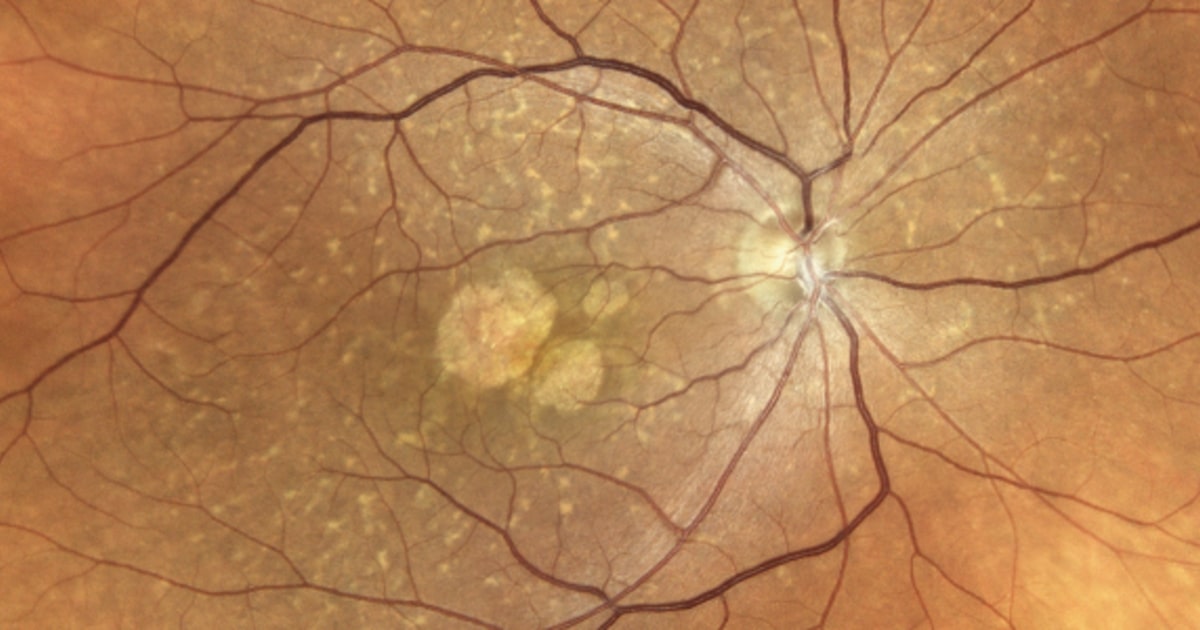
The use of color fundus photography is a relatively new tool in documenting the health of the eyes and the information it provides can help healthcare providers assess the progression of Stargardt disease. To take a fundus photo, the patient may have their eyes dilated. Next, the patient will sit in front of a low-power microscope with a small camera attached to it. The patient will place one eye in front of the camera, and the clinician will take several photos, repeating the process with the other eye. This test is painless, and it allows the specialist to see the retina, fundus, optic disc, and macula. Providers may use fundus photos to track eye health over time, and they can also be useful in the interpretation of fluorescein angiography tests.
