Ulcerative Colitis: Symptoms And Treatments
Ulcerative colitis is an autoimmune disorder in which the immune system mistakenly attacks the digestive tract. It is a form of irritable bowel syndrome affecting the innermost lining of the large intestine and rectum. Unlike Crohn’s disease, which may affect any part of the gastrointestinal tract from the mouth to anus, ulcerative colitis is restricted to the large intestine or colon. Ulcerative colitis is characterized by various degrees of flare-ups and periods of remission. Although no cure is available, treatment options are available to reduce symptoms.
10. Abdominal Pain

Pain in the lower region of the belly or the abdomen is one of the earliest signs of the disease. It tends to be present whenever the disease is active, or when there is a flare. Abdominal pain may change as the illness develops and worsens over the years. It is caused by the presence of ulcers on the lining of the colon, which become infected, inflamed and full of pus. Natural anti-inflammatory remedies are recommended as many over-the-counter medications may cause further damage to the lining of the colon.
9. Bloody Diarrhea

The presence of bloody diarrhea and mucus is an indication of a flare, or when the disease becomes active. Infected or inflamed ulcers located on the lining of the colon cause extreme irritation and disruption to the digestive process. Food that enters the gastrointestinal tract during a flare further irritates the inflamed intestines, causing diarrhea. Avoiding inflammatory foods such as dairy, wheat, gluten, fatty meats, and grains while a flare is present may reduce the amount of bloody diarrhea.
8. Fever

Fever is an indication of an infection in the body. Ulcerative colitis occurs when the lining of the colon becomes inflamed and infected, which might spike a low-grade fever. A fever will usually develop when the symptoms of the disease are not treated immediately or are allowed to get worse. The higher the temperature, the more damage is being done to the intestines. Seek immediate treatment if a fever over one hundred degrees Fahrenheit develops in addition to bloody stools.
7. Fatigue

Fatigue is a common symptom of many autoimmune diseases as the immune system is constantly in overdrive, which utilizes a lot of energy. Loss of blood is another reason why many people with ulcerative colitis experience fatigue. Getting eight hours of sleep at night may help reduce fatigue. It also helps repair and restore the immune system to a balanced state. Avoiding drinking too many caffeine beverages as this may cause further damage and irritation to the colon.
6. Weight Loss
Ulcerative colitis is common in people with digestive disorders for several reasons. First, the disruption of the gastrointestinal tract may result in an inability for the small intestine to absorb nutrients, which causes a calorie deficit. A person experiencing a flare may have no appetite or their condition may be worsened by eating or drinking, which makes it difficult to enjoy eating food. Liquid diets and vitamins may be necessary during flares to prevent malnutrition and supply the body with the energy it needs to fight the infection.
5. Anemia
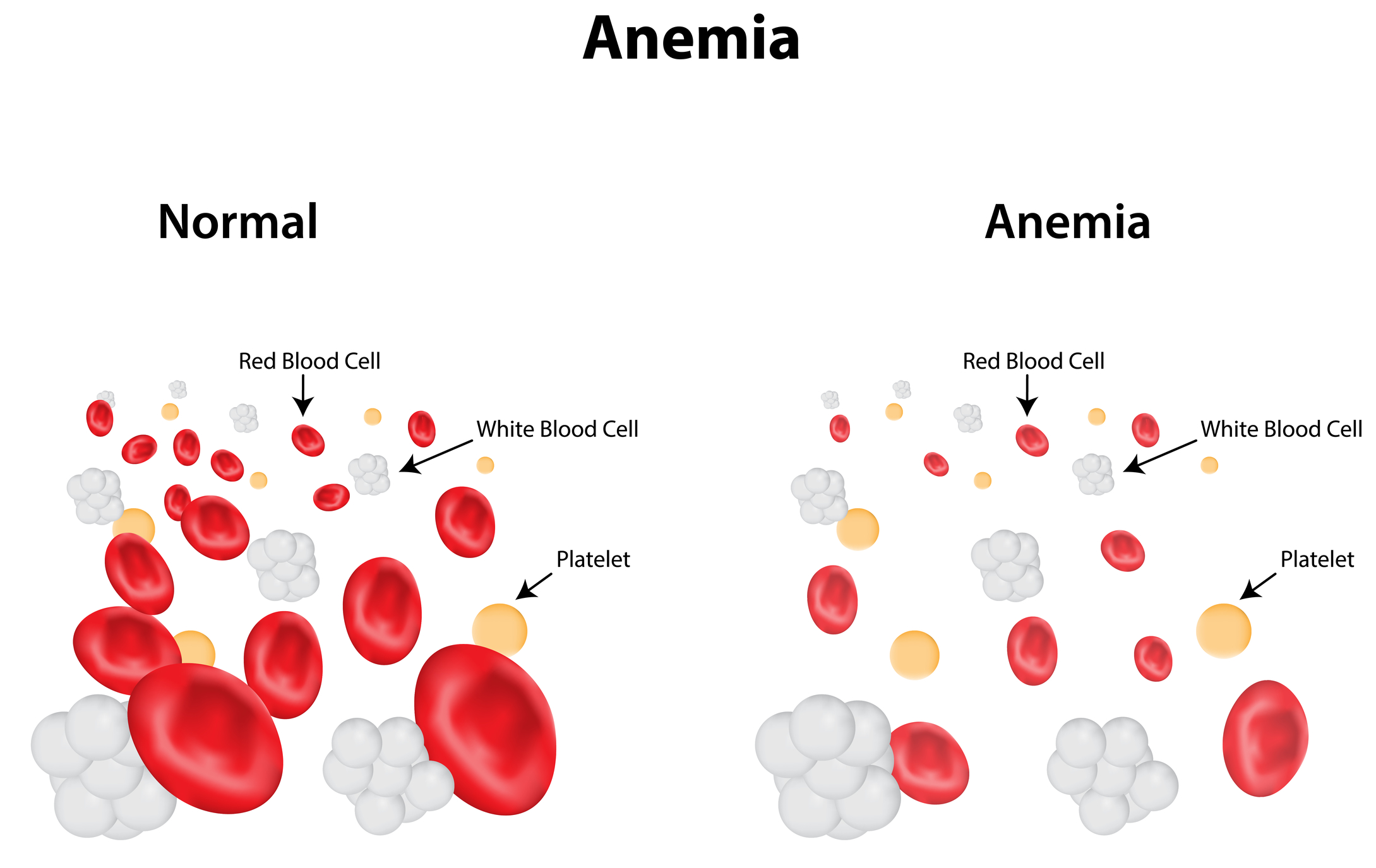
Anemia occurs when the blood is deficient in red blood cells, which are required to deliver oxygen throughout the body. Rectal bleeding and blood loss due to blood diarrhea may increase the risk of anemia. Ulcerative colitis may also cause iron-deficient anemia, which occurs when the body becomes deficient in the mineral iron. During a flare, the lining of the colon becomes infected and inflamed, which makes it difficult for the small intestine to absorb many nutrients and increases the risk of deficiencies.
4. Other Autoimmune Diseases
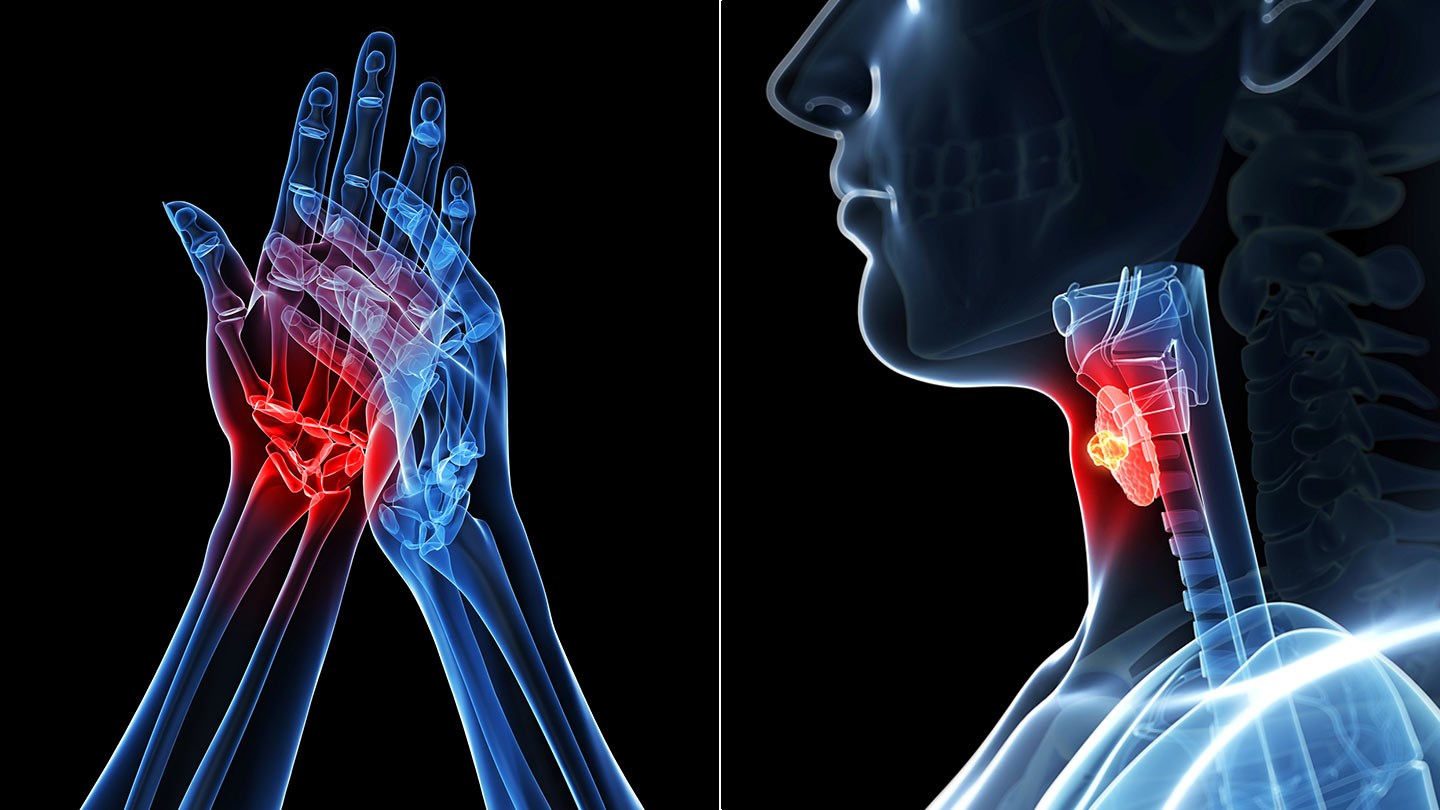
Ulcerative colitis is a form of irritable bowel disease caused by a deficient or impaired immune system; therefore, other parts of the body besides the colon may be affected. Kidney problems, bile duct and liver disease, joint problems, low back and neck pain, skin rashes, and eye pain or vision problems are common symptoms of ulcerative colitis. Autoimmune conditions tend to be related to one another, so a person diagnosed with ulcerative colitis may also be diagnosed with rheumatoid arthritis, lupus, or Hashimoto’s disease.
3. Treatment

Prescription medications such as immunosuppressant, steroid, and analgesic drugs are commonly used to treat ulcerative colitis. Severe cases of ulcerative colitis that do not respond to medication may require surgery. A colostomy is a surgical procedure in which an opening of the abdominal is created where stool can leave the intestines. It is accompanied by a colostomy bag that needs to be changed often. A colectomy is a procedure in which all or severely infected parts of the colon are removed.
2. Ulcerative Colitis Diet

Because every person with an autoimmune disease responds differently to medications and foods, there is not a specific diet recommended for all suffers of ulcerative colitis. Some people find a whole-food, plant based diet works for them while others find relief from a diet that excludes grains. An anti-inflammatory diet, or one that includes lots of fresh fruits and vegetables, has been shown to reduce symptoms of most autoimmune diseases. Keeping a journal and tracking how certain foods affect symptoms is the best way to determine the correct diet for each individual.
1. Supplements

People with ulcerative colitis may have a hard time absorbing vital nutrients; therefore, taking a whole food based multivitamin is recommended. Probiotics are “good” bacteria that help restore the health of the gut, especially after a round of antibiotics or other harsh medications. L-glutamine is an amino acid that boosts the immune system and has been shown to reduce bleeding associated with irritable bowel disease. Turmeric, Bromelain, and Boswellia are potent anti-inflammatory agents that may be able to reduce intestinal inflammation.
