Primary Sclerosing Cholangitis And How It Affects Your Liver
Primary sclerosing cholangitis is a long-term disease of the bile ducts, which are needed to carry bile from the liver to the small intestine. Bile is a digestive liquid responsible for digesting fats and the fat-soluble vitamins A, D, E, and K. Bile is made in the liver and travels through the bile ducts to the small intestine and gallbladder. Primary sclerosing cholangitis is similar to primary biliary cirrhosis with a few key differences. Both conditions cause liver damage.
10. What Is Primary Sclerosing Cholangitis?
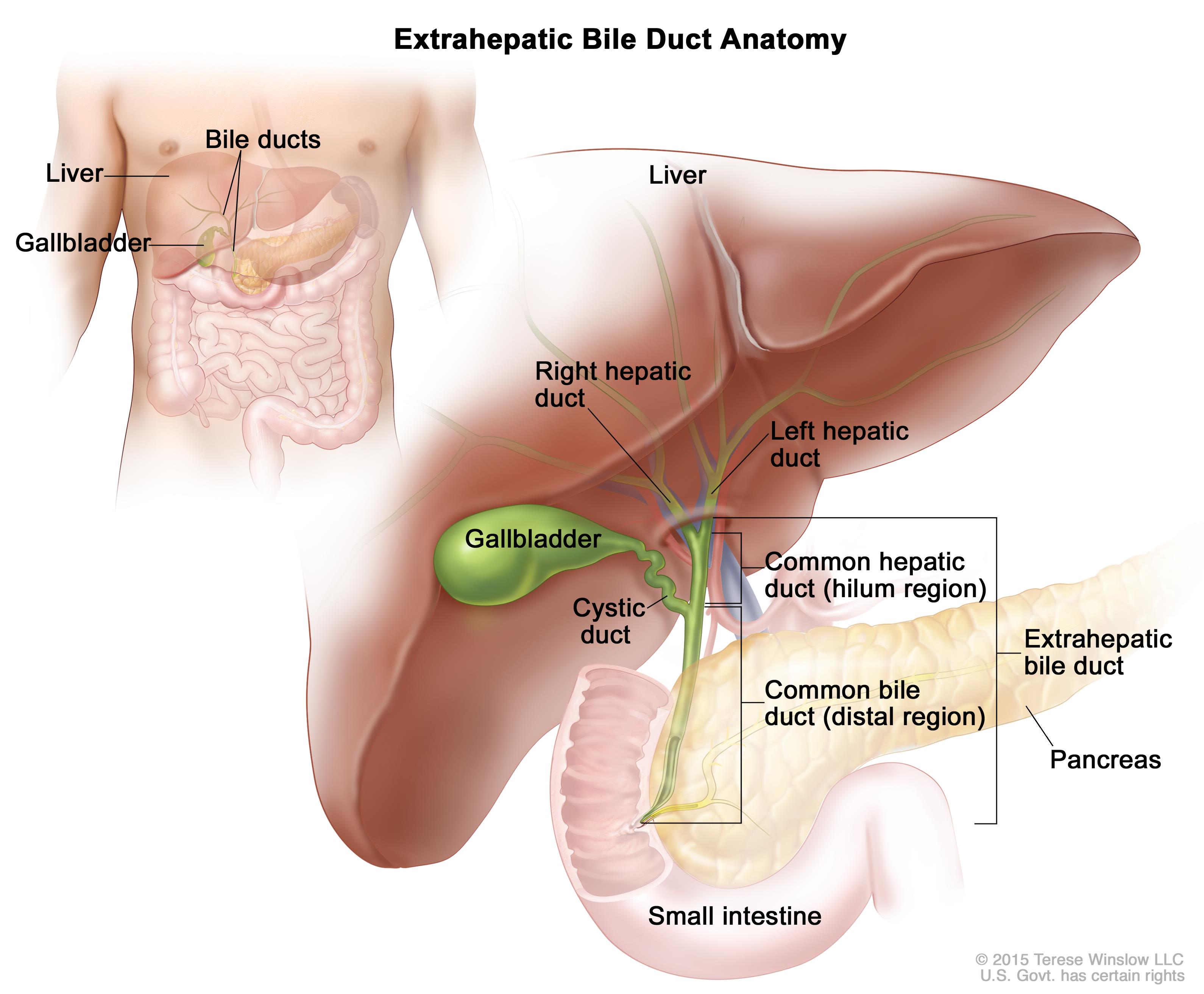
People with primary sclerosing cholangitis experience blocked bile ducts due to scarring, inflammation or fibrosis, which causes bile to build up in the liver instead of traveling to the small intestine. This buildup of bile causes damage to liver cells, and eventually, cirrhosis of the liver develops. Cirrhosis increases the amount of scar tissue in the liver, which causes the liver to slowly shut down by blocking drainage of the bile ducts and causing infection of the bile.
9. Prognosis
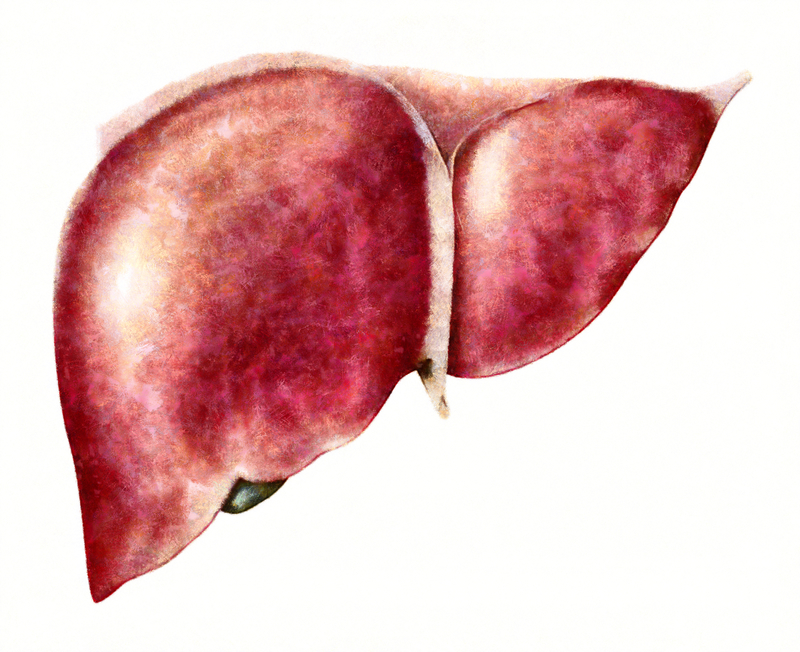
Primary sclerosing cholangitis progresses very slowly over the course of many years before symptoms develop. Symptoms may then remain stable or consistent, they may gradually progress, or they may come and go. According to the American Liver Foundation, liver failure may occur anywhere from ten to fifteen years after diagnosis, and sometimes longer. Because of this, most people with primary sclerosing cholangitis will eventually need a liver transplant. Primary sclerosing cholangitis may also result in bile duct cancer.
8. Symptoms

Symptoms of primary sclerosing cholangitis may not show up until after a diagnosis has been given due to a routine blood test or if an X-ray shows abnormalities in the liver. Early signs may include itching and fatigue, although some people may go years before developing any indication of disease. As the illness progresses, the following symptoms may occur: fever, chills, night sweats, pain in the upper right abdomen area, weight loss, an enlarged liver, yellowing eyes and skin (jaundice), and weight loss.
7. Causes And Risk Factors
Although it is not clear what causes primary sclerosing cholangitis, researchers at the Mayo Clinic indicated that the condition might be triggered by to an immune system reaction to a toxin or infection in people who are predisposed to the condition. The American Liver Foundation stated that approximately seventy percent of people with primary sclerosing cholangitis are men. Individuals who have been diagnosed with primary sclerosing cholangitis are often diagnosed with Crohn’s disease or ulcerative colitis as well.
6. When To Seek Help

Seeking treatment is difficult as many symptoms do not appear for years. Talk to a doctor if there is unexplained general itching all over the body that persists no matter how much scratching or treatment is done. Feeling extremely fatigued all the time is another good reason to seek help. People who have already been diagnosed with Crohn’s disease or ulcerative colitis may want to talk with their doctor about primary sclerosing cholangitis to monitor liver health over the years, especially if unusual or increased symptoms develop.
5. Primary Sclerosing Cholangitis Versus Primary Biliary Cirrhosis
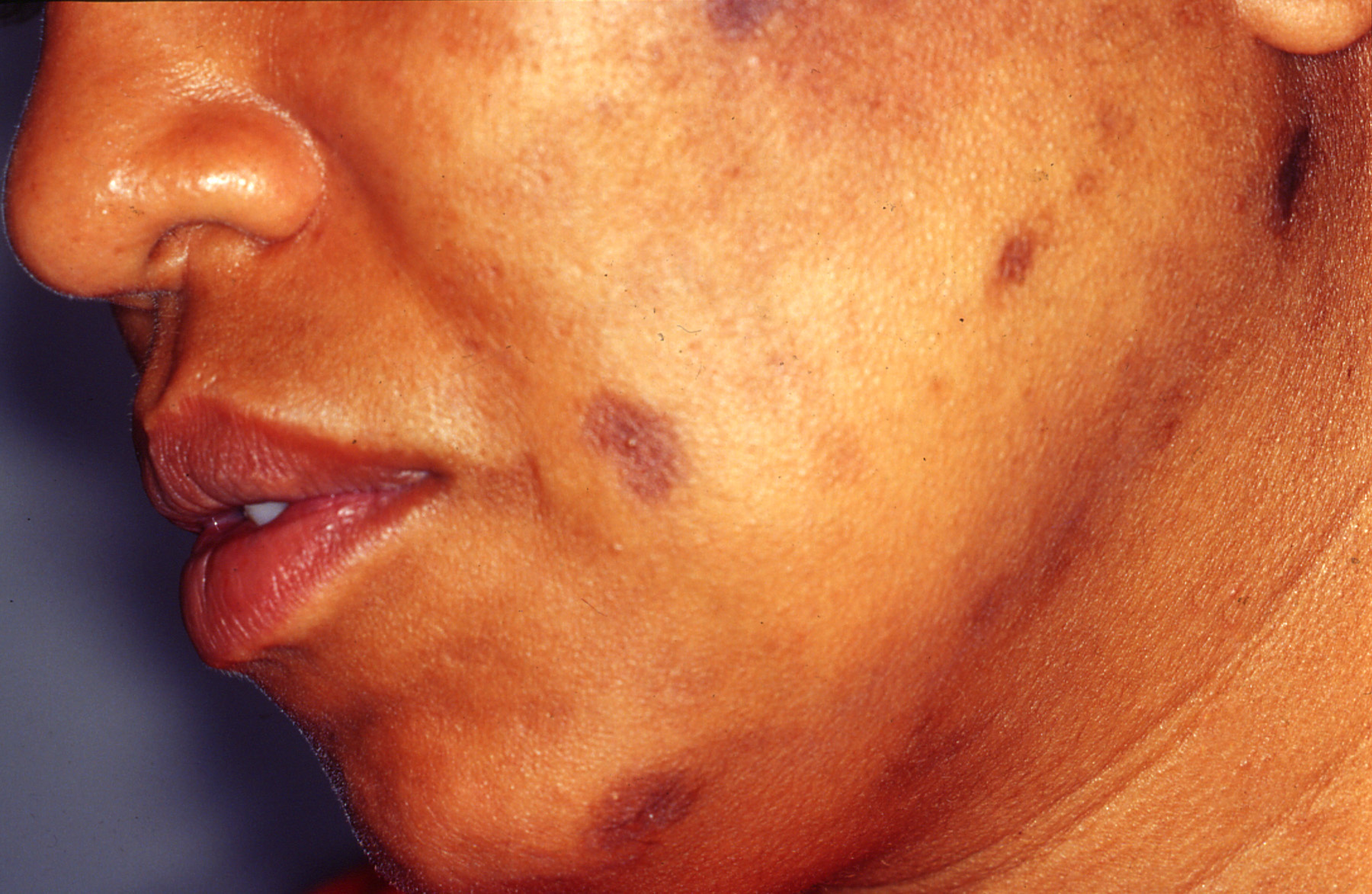
Primary sclerosing cholangitis and primary biliary cirrhosis are similar conditions that cause severe liver damage and can be hard to differentiate. According to a study published in the journal Gastroenterology, “destructive cholangitis occurs in both diseases and leads to similar clinical and biochemical abnormalities.” The study showed that primary biliary cirrhosis mostly occurred in middle-aged women who were hyperpigmented and had keratoconjunctivitis sicca (dry eye) while primary sclerosing cholangitis occurs in young men who experienced symptoms of fatigue and frequently had chronic ulcerative colitis.
4. Complications

Complications of primary sclerosing cholangitis may eventually lead to liver failure or liver disease, frequent viral and bacterial infections, bile duct cancer, thinning bones or low bone density, and colon cancer. Primary sclerosing cholangitis may also cause portal hypertension, which occurs when the portal vein that is responsible for delivering blood from the digestive system to the liver leaks fluid from the liver into the abdominal cavity. Portal hypertension can also divert blood flow from the portal vein to others, which increases blood vessel swelling and can be life-threatening.
3. Treatment

No cure or specific treatment is currently available for primary sclerosing cholangitis; however, it is strongly advised to monitor the progress of the disease by seeking care from a medical professional. Medications are available to help cope with the itching associated with the disease and antibiotics may be needed to treat bile duct infections as they develop. Bile duct surgery or an endoscopy can be used to improve bile flow temporarily. In most cases, a liver transplant will be needed.
2. Preventative Care

Because there is no cure for primary sclerosing cholangitis, it is important to take precautions against the disease before it causes irreversible damage. According to a study published in The Journal of General Internal Medicine, preventative care plays a significant role in patients with chronic liver conditions. Results showed that avoiding alcohol, the hepatitis vaccination, nonsteroidal anti-inflammatory drugs (NSAIDs), and iron supplementation may help protect the liver. A low-fat diet or one that is high in “good” monounsaturated fats may also help.
1. Natural Remedies For Liver Support

Replacing certain “bad” foods, such as alcohol, sugary drinks, refined carbohydrates and sugar, and processed foods, with “good” foods including raw vegetables, ginger root, bananas, sweet potatoes, milk thistle, and dandelion root, has been shown to improve liver function. Supplementing with vitamin E, black seed oil, and turmeric may also reduce inflammation and improve liver function. According to the Global Healing Center, the following foods have been shown to cleanse the liver: garlic, beets, green tea, carrots, green leafy vegetables, olive oil, avocados, and apples.
