7 Tips For Managing Eczema In The Winter
As the winter season approaches, spend a little time understanding how to care for the largest organ of the human body, inside and out. Cold months are particularly difficult for patients with eczema because the dry, frigid conditions dramatize the symptoms so severely. Before tackling the most irritating signs of cold weather, take a look at the condition itself and at the many variables that control its manifestation. According to extensive research, the body must be balanced both internally and externally for eczema to be conquered at its best and worst.
A Brief Overview: What is Eczema?

Patients who experience itchy, inflamed, dry skin may suffer from eczema or atopic dermatitis, as itis known in the medical community. Just a step below psoriasis, eczema is a condition that makes the skin more sensitive to everything because it weakens the skin as a barrier to stressors like germs. Research has revealed that skin afflicted with eczema does not generate enough filaggrin, a structural protein that keeps moisture locked in the epidermis. As few as four years ago, studies began referring to eczema as having pathogenic factors, meaning that the skin has difficulty repelling bacteria and other microorganisms and reacts accordingly. The good news is that both internal and external solutions can be applied for relief.
Go With Your Gut

Because the body can become compromised by environmental stressors, it is essential for patients with eczema to maintain strong internal health. The National Eczema Association confirmed that the first approach should be a probiotic, which contains a collection of good bacteria strains the body needs to cut back on bad bacteria. Though the probiotic courses through the intestines, it supports immune function necessary for both treating and preventing a flare-up. Remember staph infections? The bacterium Staphylococcus occurs in abundance on the top layer of the skin; when it occurs too abundantly, the result is a dangerous infection. By taking a probiotic supplement once a day, especially during winter, the skin is less likely to become inflamed from an infection.
Winter as a Stressor

In a 2001 volume of the International Journal of Biometeorology, eczema-afflicted patients in Davos, Switzerland were observed under fifteen different meteorological conditions. The study found that in patients with atopic eczema, a certain range of thermo-hygric atmospheric conditions with a balance of heat and water loss on the skin surface is essential for the skin to feel comfortable. In layman’s terms, the skin feels best when the climate is appropriately balanced. As the temperature drops, humidity drops with it. Through the process of osmosis (the movement of water molecules to balance hydration), skin dries out when it makes contact with even drier air. Since eczema already causes dry skin, contact with dry air exaggerates this discomfort. Therefore, it is essential to use topical products that both replenish the skin’s moisture and aid in moisture retention.
What Do Doctors Say About Moisturizers?

Moisture and anti-inflammatory creams are key. Researchers at Johns Hopkins University have extensively studied eczema treatments, and they recommend a hydrocortisone cream in place of regular lotion. In addition to its moisture contents, hydrocortisone has a steroidal anti-inflammatory agent that soothes the skin and aids in healing. Apart from using cream, the Johns Hopkins guide recommends using a petrolatum-based ointment that, rather than being entirely absorbed by the skin, sits on the surface of the skin and acts as an artificial barrier. The National Eczema Association also recommends a skin barrier cream infused with lipids and ceramides that imitate those naturally found in skin. When those elements are well-stocked, moisture is locked in, and the symptoms of eczema lessen significantly.
Investing in a Humidifier

Looking back on the study in the high mountains of Davos, Switzerland, researchers seemed to suggest that eczema-prone skin requires an optimal climate. However, since eczema patients cannot simply move to a better climate, they should at least use a humidifier in their home during winter. A humidifier takes in dirty, dry air and returns it as clean, moist air. The body heals during sleep, so when an eczema patient controls their environment during sleep, the skin can both heal properly being protected from further dehydration. Additionally, a humidifier that simultaneously acts as an air purifier can cut out allergens and toxins that cause harm to compromised skin. As an even simpler solution, patients should drink plenty of water throughout the day.
Wet-Wrap Therapy
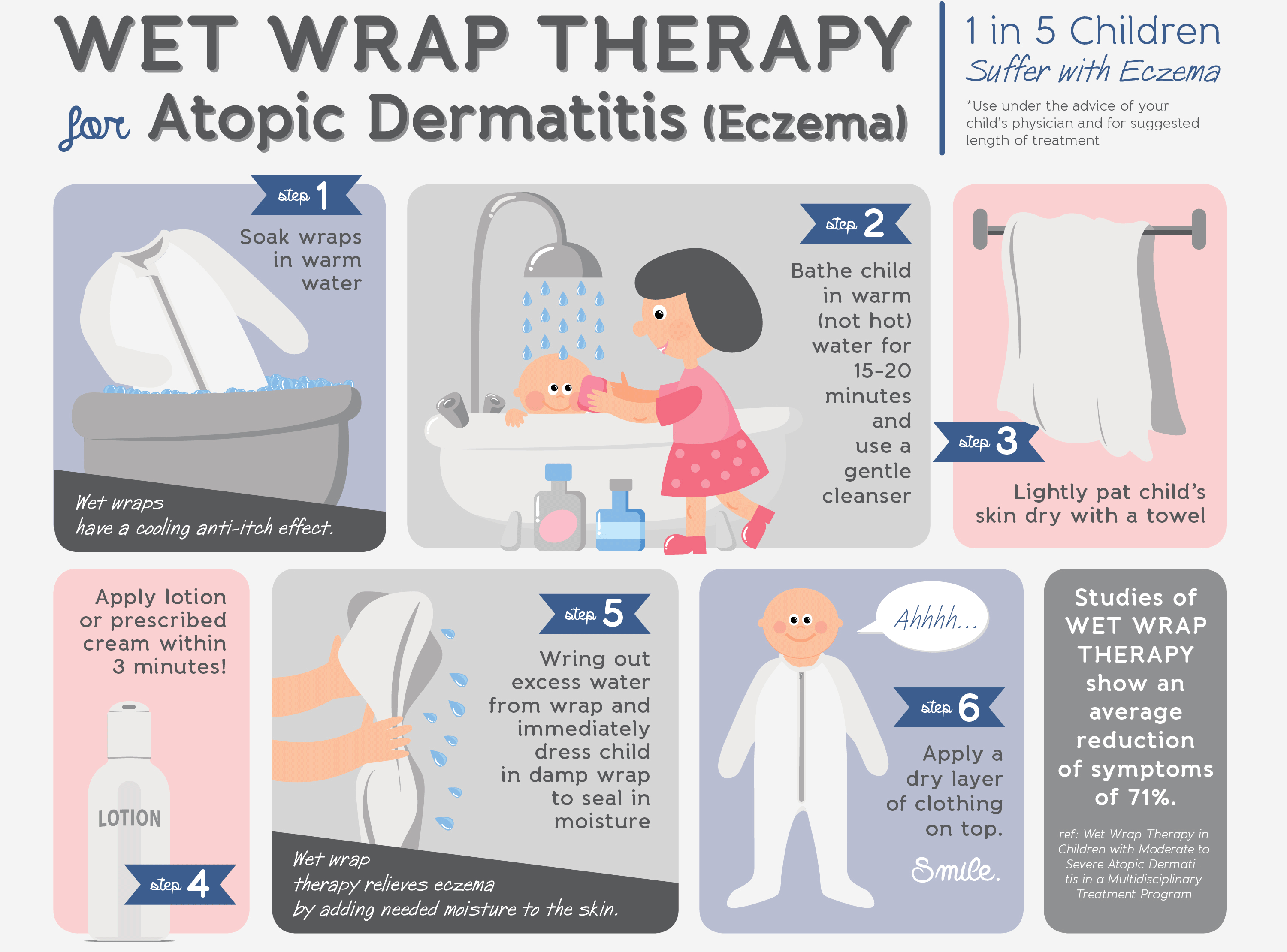
Seattle Children’s Hospital mentions wet-wrap therapy as a solution for severely dry skin prone to eczema; imagine the process as a pair of pajamas equipped with their own humidifier. The wet wraps seal in moisture to the skin to do a number of things: keep moisture from seeping back out, increase the effectiveness of topical steroids for healing, and provide a barrier against scratching. It is recommended to use wet-wrap therapy only in severe cases, and it should only be done a few days at a time. The purpose is to calm a flare-up, rather than prevent one. If patients with an eczema flare-up have to face the cold during the day, this might be an essential part of their nightly routine.
Look Near, Look Far

For further solutions, it is advisable to look at research done in countries who have winter down to a science. Centers in places like Iceland have used geothermal technology to heal skin diseases, while the Swedish Medical Center promotes anything from St. John’s Wort to Calendula and Chamomile as topical soothing agents. Norwegian researchers encourage baths with potassium permanganate. Paul Hazelden, who has suffered from eczema since infancy, swears by Finnish saunas (though such saunas are available elsewhere). Danish dermatologists look at the relationship between eczema and food; particularly dairy and gluten. Overall, medical researchers in Scandinavia stress that eczema is best treated using a combination of methods that make the body whole on the inside and out. Though these treatments may not be as conventional as an over-the-counter hydrocortisone cream, there is plenty of research to prove the effectiveness of the other topical creams, diet alterations, and other methods mentioned.
Conclusion

During any time of the year, eczema can be debilitating because of the distracting itch and constant pain. There is ample research to prove that the winter months create dry conditions that pull precious moisture from the skin and exaggerate symptoms. However, the internal state of the body can change at any point during the year. As stated above, eczema patients have the best chance of recovery during the coldest season when they combine several internal and external methods and use them according to the severity of their condition. By doing these things as they apply to a specific case of eczema, it is possible to both heal and protect eczema-prone skin from the harshest climates. Instead of dreading the cold weather and the pain it brings, master eczema using these tips and enjoy the best the winter season has to offer.
