Causes and Treatments of Childhood Bedwetting
Bedwetting is an embarrassing condition affecting millions of children and teenagers each year. Approximately fifteen percent of children will continue to wet the bed after the age of five. Although ninety-five percent of children over the age of ten are dry at night, some will continue to wet the bed well into their teen years. According to Doctor Howard Bennett, pediatrician, and author of Waking Up Dry: A Guide To Help Children Overcome Bedwetting, “I call it the hidden problem of childhood. Unlike asthma or allergies, it’s just not talked about outside the house.” Here are some possible causes and treatments.
10. There Is No Single Cause

Bedwetting can be an embarrassing situation for children, especially those who are teased by their siblings or are scared to invite friends over to spend the night. But for many kids, it is beyond their control. According to Bennett, “Ninety percent of kids think they're the only ones who wet the bed, which makes them feel even worse.” Although there is no single cause of bedwetting in children and teens, Bennett states it may be an inevitable part of growing up for some kids and is not due to laziness.
9. Bedwetting Gene

Research suggests that bedwetting may be attributable to a particular genetic predisposition. Children with relatives who wet the bed are more likely to experience the same fate. “The majority of bedwetting is inherited. For three out of four kids, either a parent or a first-degree relative also wet the bed in childhood,” says Bennett. Scientists have determined specific genes on chromosomes eight, twelve, and thirteen to be responsible for delayed nighttime bladder control. Bennett suggests informing a child of these genes as it helps kids feel like they are not alone and it is not their fault.
8. Delayed Bladder Maturation

While genetics may play a role in bedwetting, it is not the only factor. Some children may experience a delay in the maturation of their bladder, making them prone to bedwetting at night. Bennett says, “Simply put, the brain and bladder gradually learn to communicate with each other during sleep, and this takes longer to happen in some kids.” A child’s ability to control their bladder at night is as unique as other growth characteristics and may take some time to develop fully.
7. Low Anti-Diuretic Hormone (ADH)

The anti-diuretic hormone, or ADH, is a hormone that tells the kidneys to produce less urine. Also known as arginine vasopressin, the hormone is made in the hypothalamus and stored in the posterior pituitary gland. Its primary function is to regulate and balance the amount of water in the blood. Studies show that children who wet the bed have lower amounts of ADH at night. Blood tests can be done to determine if a child is low in ADH.
6. Deep Sleeping

Bedwetting in children may be due to a sleep disorder. According to Bennett, “Families have been telling us for years that their children who wet the bed sleep more deeply than their kids that don’t. Some of these children sleep so deeply that their brain doesn’t get the signal that their bladder is full.” Doctor John Kryger, pediatric urologist at American Family Children’s Hospital in Madison, confirmed the link by stating, “Practically every bed wetter I see is a deep sleeper, and when children go into a deep sleep, brain patterns change and affect bladder control.”
5. Underdeveloped Functional Bladder

While a child may have a normal sized bladder, it may not be functionally fully developed. A child who wets the bed may have a weak functional bladder, which sends mixed signals to the brain that it is full when it is not. This may cause the brain to signal the release of urine. “A large part of the problem is a delay in the maturity of the central nervous system and interaction between the child’s brain, sleep patterns, and bladder-control center,” Kryger says.
4. Constipation

A child who is constipated may wet the bed due to an increase in pressure on the bladder from fecal matter in the digestive tract. Full bowels press on the bladder, causing contractions during activities such as walking or sleep. Bennett says, “This is the one that's hiding in the background. Once kids are toilet trained, parents often don't know how often a child is going, they are out of the 'poop loop.’” Increasing a child’s dietary fiber can help alleviate constipation.
3. Treatment

Kryger states that the best way to reduce the risk of bedwetting is to avoid drinking fluids one hour before bedtime. Another useful method is to reduce caffeine intakes such as in soda or energy drinks. Kryger also recommends cutting back on eating food too late at night, so the bowel does not feel full and press on the bladder during sleep. Allowing for proper time to have a bowel movement during the day is an important part of alleviating constipation.
2. Underwear Alarm
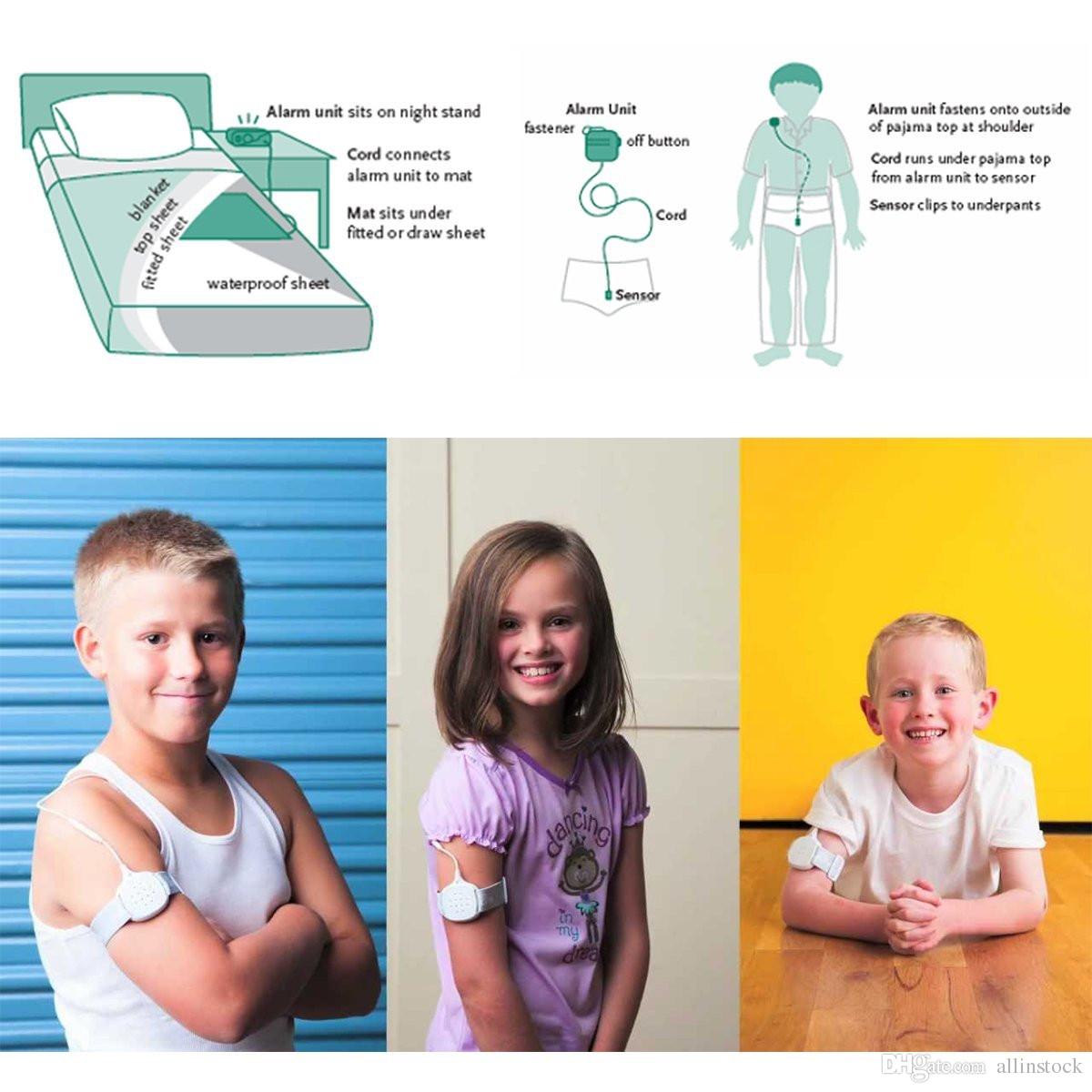
An alarm attached to the child’s underwear may help if all other options fail. Of the alarm, Kryger says, “When it gets wet, the alarm vibrates or rings, so the child is startled from sleep. Over time, the fullness of the bladder awakens the child before the alarm goes off. It’s a principle that involves conditioning the body to awaken when the bladder is full.” According to Kryger, the underwear alarm helps cure more than sixty percent of bet wetters but can be a nuisance.
1. Medications

The most commonly used drug for bedwetting in children is called desmopressin, which is a hormone that tells the kidneys to retain urine. It has a sixty percent cure rating in children who wet the bed. Kryger says, “There are virtually no side effects, and for the fortunate ones, it may work overnight. Some may use it for special occasions like sleepovers, camping trips, and not worry about the bedwetting other days of the week.”
