The Dangers Of Deep Vein Thrombosis
Deep vein thrombosis, also known as thromboembolism and postphlebitic syndrome, is a critical and sometimes fatal blood condition that occurs when blood clots form in various parts of the body, typically in a leg or the lower half of the body. There are specific signs and symptoms patients need to be aware of, especially if they are at high risk of developing blood clots due to genetics or their lifestyle. Start reading to discover what causes this severe condition, its symptoms, the fatal complications it can lead to, and how individuals can prevent it.
What Is Deep Vein Thrombosis?
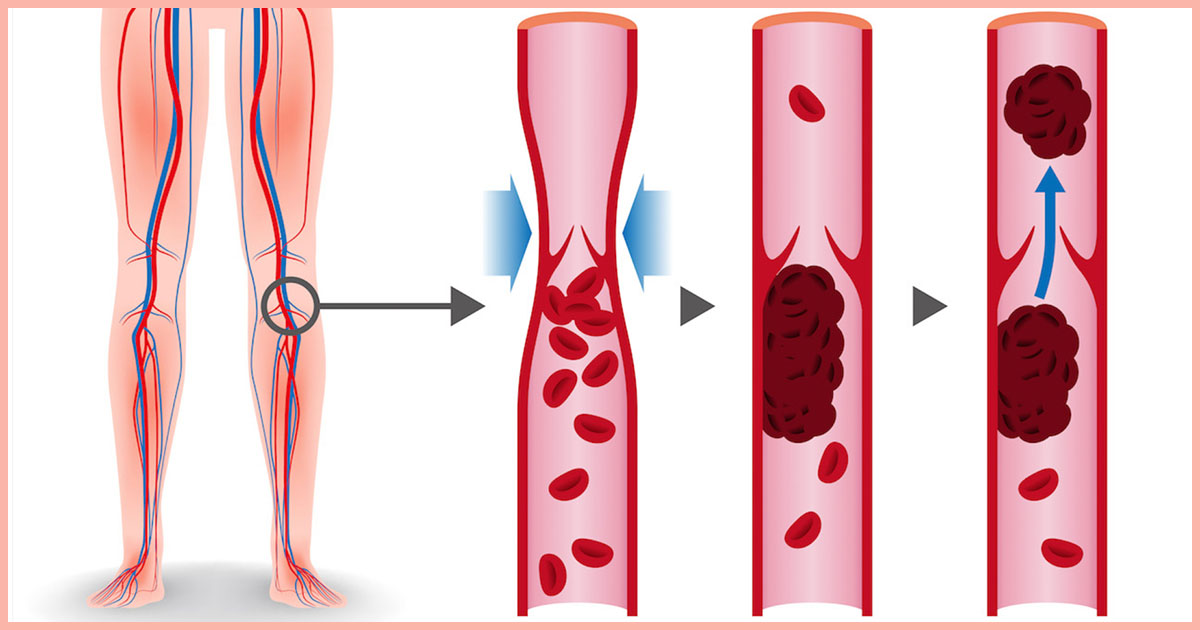
Deep vein thrombosis, also known as DVT, occurs when a thrombus, commonly called a blood clot, forms in one or more of the deep veins within the body, particularly in the legs, thighs and lower extremities, though it can also occur in other parts of the body. A blood clot is a clump of blood in a gelatinous, solid state that blocks blood from flowing freely due to its size. This condition can result in leg pain or swelling, however, it is common for a patient to not experience noticeable symptoms, and DVT will only become apparent once a pulmonary embolism occurs. Deep vein thrombosis can become severe and even fatal, as the blood clots in the veins may break loose, travel through the bloodstream, and become embedded in the lungs, blocking blood flow, resulting in a pulmonary embolism.
Signs & Symptoms To Be Aware Of

Typical symptoms and signs of deep vein thrombosis include swelling and acute pain in the affected leg that often starts in the calf and can feel like cramping or tenderness, red or discolored skin in the affected area, and a feeling of intense warmth in the affected area. According to the National Heart, Lung, and Blood Institute, additional common symptoms include swelling of a foot or ankle, and severe, unexplained pain in the foot and ankle. These symptoms usually only occur in about half of the individuals who have the condition, as the other half does not show any visible signs.
