11 Options For Treating Barrett's Esophagus
Barrett’s esophagus may not cause noticeable symptoms on its own, but it carries serious implications that shouldn’t be ignored. Often developing as a complication of chronic gastroesophageal reflux disease (GERD), this condition causes the lining of the esophagus to change, resembling the tissue typically found in the intestines. While these changes are subtle and silent, the risks they bring—including an increased chance of esophageal cancer—are anything but. GERD-related symptoms like frequent heartburn, chest discomfort, and trouble swallowing often go hand-in-hand with Barrett’s esophagus, serving as red flags for potential trouble beneath the surface. Early detection and routine monitoring are crucial, especially when it comes to spotting precancerous cells that are far more treatable when caught early. To help you better understand the warning signs and prioritize your digestive health, we’ve expanded our list to 11 important symptoms and red flags associated with Barrett’s esophagus. Recognizing these signs early can lead to faster diagnosis, more effective treatment, and better outcomes overall.
1. Endoscopic Resection

Endoscopic resection is a method used to remove early-stage cancer cells and precancerous cells from the digestive tract lining. This option is an ideal alternative to traditional surgery that is sometimes used to remove precancerous and cancerous growths in the digestive tract lining. The reason for this is because endoscopic resection is considerably less invasive and less risky. This procedure is helpful for patients with Barrett's esophagus because it allows for any concerning tissues to be removed from the abnormal esophageal lining. It is imperative that these tissues are immediately extracted to stop the progression of cancerous or precancerous growths in the esophagus lining. The procedure is performed using an endoscope or a long thin flexible tube with a video camera and a light on the end of it. The surgeon inserts the endoscope into the individual's mouth, down their throat, and into their esophagus. Once located, the area of concern is carefully removed by maneuvering specialized instruments through the tube. Usually, medication is used to sedate the patient, and a numbing solution is used to ensure that they do not feel any pain or discomfort during the endoscopic resection. Most patients can return to their normal activities the next day.
2. Radiofrequency Ablation
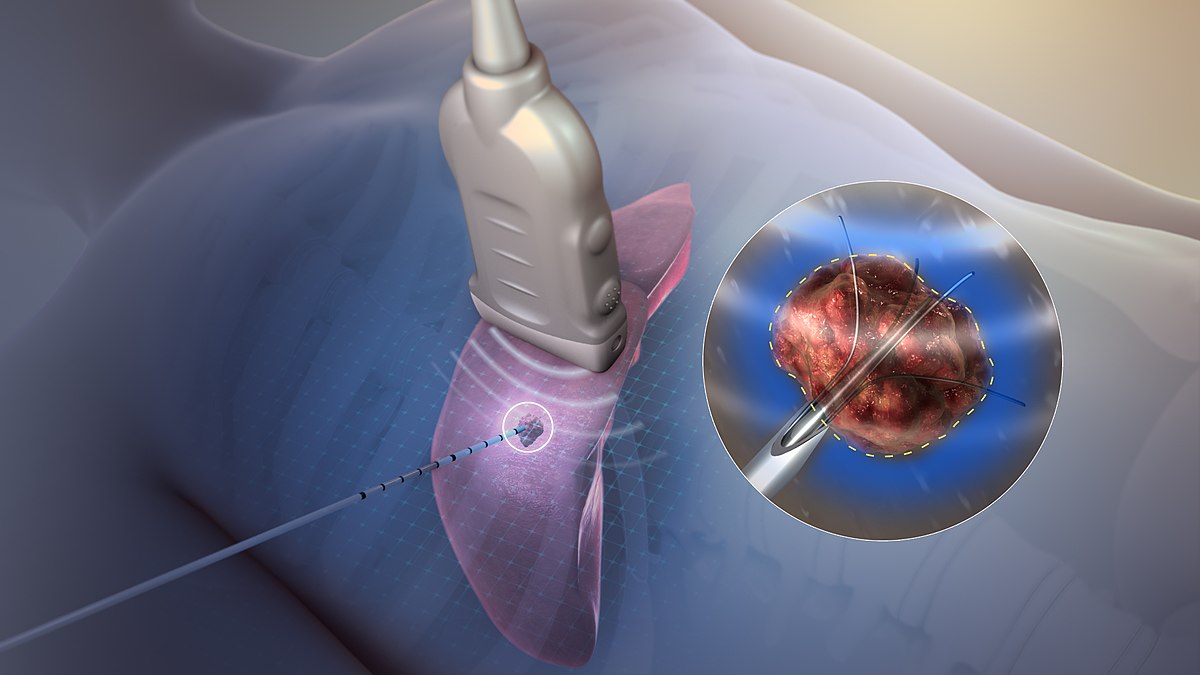
Radiofrequency ablation is a procedure used to ablate diseased or abnormal tissues in the digestive tract with the use of heat energy. Tissue ablation is performed so the abnormal tissue can be destroyed to give the body an opportunity to grow back new healthy tissues in its place. Radiofrequency ablation allows Barrett's esophagus patients to eradicate the abnormal lining of their esophagus. The procedure is carried out with the use of an endoscope similar to the one used in an endoscopic resection. However, the endoscope in radiofrequency ablation has an electrode on the end of it. The electrode is the device that will deliver heat energy directly to the abnormal tissues of the esophageal lining. Once the application of heat is administered to all of the diseased tissues, they will slough off between two and three days following the procedure. It will take the individual around six to eight weeks to regrow normal squamous cell lining in their esophagus. Depending on the extent of Barrett's esophagus, up to three separate radiofrequency ablation treatments may be required to remove all of the diseased tissues in the esophageal lining.
