15 Causes of Cervical Dystonia You Need to Know About
Cervical dystonia—also called spasmodic torticollis—is more than a rare muscle condition. It’s a deeply disruptive neurological disorder that twists the neck into painful, uncontrollable positions, often leaving patients in daily discomfort and confusion. A tilted head, a raised shoulder, a chin that won’t stay still—these aren't just symptoms; they’re signs of a body fighting itself. But why does it happen? That’s the question we’re tackling head-on. In this expanded list of 15 Causes of Cervical Dystonia You Need to Know About, we break down the wide range of triggers—from genetics to injuries, medications to neurological disorders. Some causes are inherited. Others are triggered by trauma, medication, or even chronic misdiagnosis. And while not all are preventable, understanding the full landscape of possible causes can be the first step toward managing—and reclaiming—control. If you've been searching for clarity, start here. The causes are more layered than you think.
1. Family History And Genetics
Genetics and family history appear to play a role in some cases of cervical dystonia. Researchers estimate between ten and twenty-five percent of cervical dystonia patients also have a family history of the condition. The condition is estimated to affect around sixty thousand individuals in the United States, so up to fifteen thousand of those have a family history of it. Genetics may increase an individual's chances of developing cervical dystonia, but researchers believe genetics alone are not responsible. Instead, genetics are combined with a variety of environmental and physical factors to increase the risk of developing cervical dystonia. Researchers have discovered cervical dystonia tends to present in individuals who have mutations in one or more of several genes. Gene mutations linked to cervical dystonia have been identified in the ANO3, CIZ1, THAP1, and GNAL genes. With that said, not enough information is currently available about how the mutations affect an individual's chances of developing cervical dystonia. Because of this, there is no way to do a genetic test for diagnostic purposes with cervical dystonia, and the condition must be assessed through symptoms and family history alone.
2. Certain Injuries
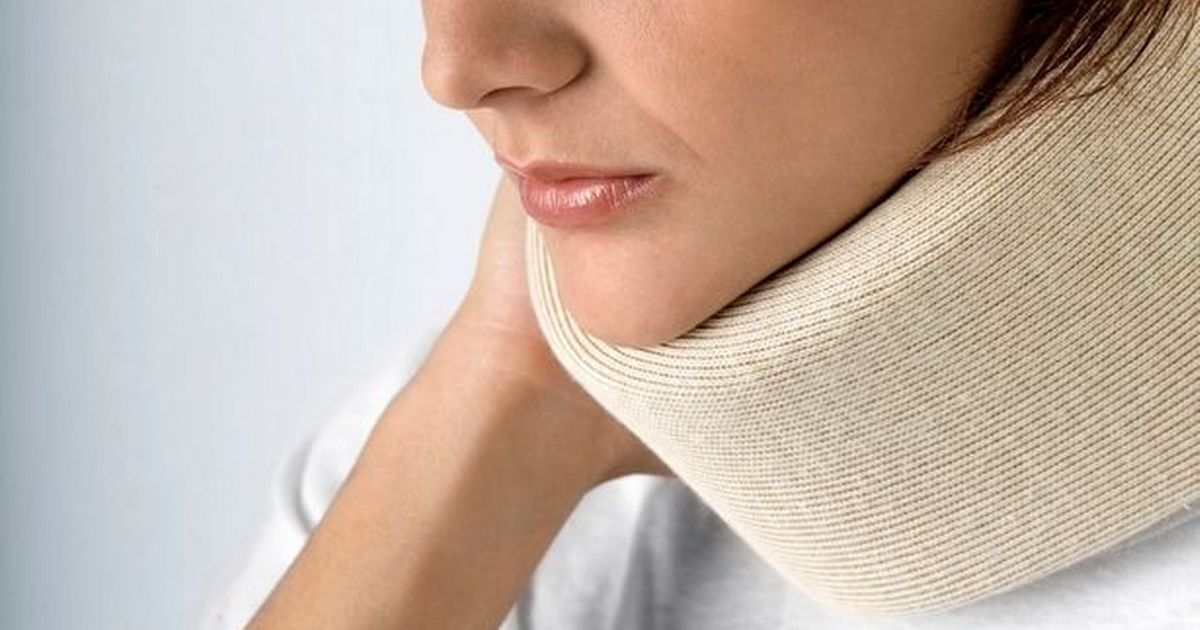
Certain injuries may cause an individual to develop cervical dystonia. In cases where there's an underlying cause like an injury or neurological disorder, the condition is called secondary cervical dystonia. Injuries to the shoulders, neck, or head increase the likelihood of an individual developing cervical dystonia. This may be considered a kind of post-traumatic dystonia, which is dystonia that occurs after an injury or trauma to the affected body part. The most common injury leading to cervical dystonia is whiplash, which some individuals experience in car accidents or when suffering impacts at sporting events. Whiplash occurs when the head snaps quickly backward and forward in a way that causes muscle injury. If individuals suspect they have suffered a whiplash injury, they should have their neck evaluated to make sure no damage was done to their spine. It's important to be attentive during the rehabilitation process for an injury. If patients notice they're developing symptoms of abnormal tension or spasticity, they should talk to their doctor to see if there are ways to mitigate it.
