Key Points to Know About Living with Diverticulitis
Diverticulitis isn’t just uncomfortable—it can be confusing, unpredictable, and downright disruptive. But the more you understand it, the more power you have to manage it. This condition starts with tiny pouches (diverticula) that form in your colon—often silently, without symptoms. But when they become inflamed or infected, the result is diverticulitis, a painful gastrointestinal flare-up that can bring abdominal cramping, fever, nausea, or sudden changes in digestion. It can feel alarming—but it doesn’t have to be unmanageable. The key is knowing what to watch for, what triggers to avoid, and what treatment paths are available. Whether you’ve just been diagnosed or you’re trying to prevent a recurrence, knowledge is your best ally. That’s why we’ve expanded our guide to 27 essential symptoms, causes, and treatments—to give you a clear, comprehensive roadmap for recognizing early signs, taking action, and protecting your gut health for the long haul. Let’s break it down.
1. Causes Of Diverticulitis
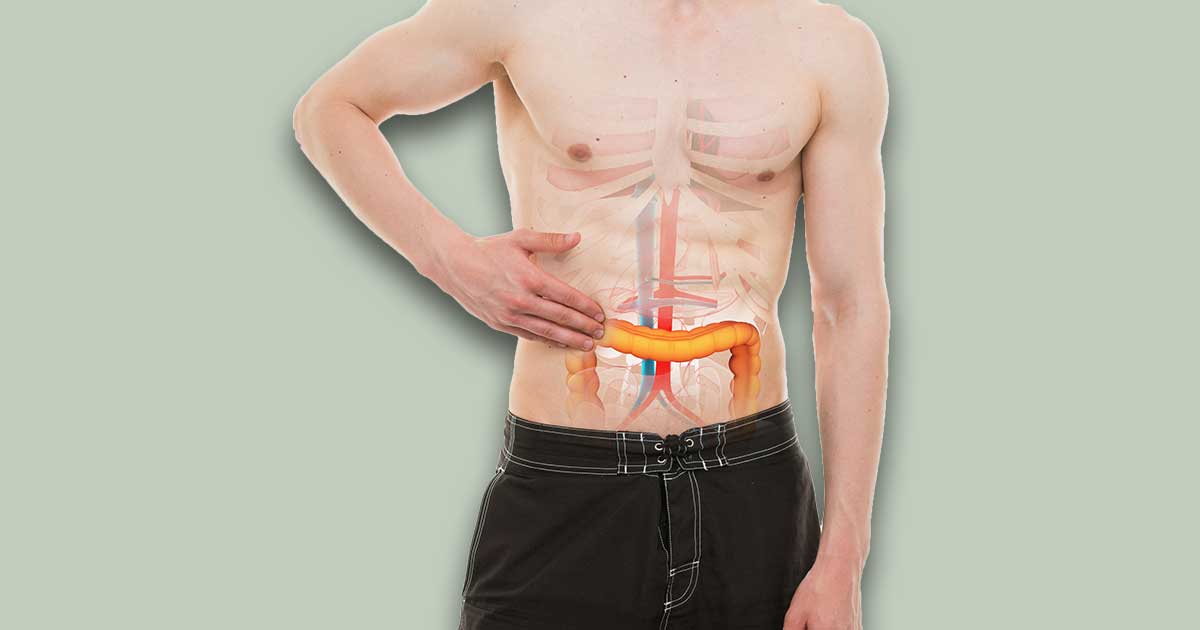
Diverticulitis does not always occur in everyone who lives with diverticula. When a person has these nodules in their colon, it is not a guarantee they will become inflamed or infected; this only occurs if there is too much pressure on the colon. These pockets are weak, and any amount of pressure can cause one to tear or in more severe cases, burst. This causes inflammation and can cause an infection depending on how much bacteria are able to make their way into the torn diverticula. Inflammation due to pressure does not always equal an infection, but it does increase a patient’s likelihood of developing an infection.
2. Pain In The Abdomen

One of the most prevalent signs of diverticulitis is a pain in the abdomen on the left side of the bodythat lasts longer than several days. It is not nearly as common on the right side of the body, but that does not mean it will not ever occur on the right side. Ethnicity, diet, and other factors play a significant role in the development of diverticulitis on the right side. If this pain lasts longer than a day or two, it is more likely a symptom of diverticulitis than a more common issue such as an upset stomach or constipation.
