5 Stages of Chronic Kidney Disease: Everything You Need to Know
Chronic kidney disease (CKD) is a silent but serious condition that gradually reduces the kidneys' ability to filter waste and excess fluids from the blood. Because symptoms often don’t appear until the disease has significantly progressed, many people are unaware they have it until complications arise. CKD is closely linked to diabetes, high blood pressure, and heart disease, making it a widespread health concern that affects millions. If left untreated, it can lead to kidney failure, requiring dialysis or a transplant to sustain life. Understanding CKD is the first step in managing it effectively, which is why we’ve expanded our guide to cover everything you need to know—from early warning signs and risk factors to diagnosis, treatment options, and lifestyle changes that can slow its progression. Whether you’ve been diagnosed, are at risk, or want to learn more, this comprehensive guide will equip you with the knowledge to face CKD with confidence and take proactive steps toward better kidney health.
Stage One: The Silent Warning Sign
At stage one of chronic kidney disease (CKD), the kidneys are still functioning almost normally, and most patients experience no noticeable symptoms. However, beneath the surface, small but significant changes may already be happening. A patient is classified as having stage one CKD if their estimated glomerular filtration rate (eGFR) is 90 or higher, but there are signs of kidney damage, such as protein in the urine (proteinuria) or structural abnormalities detected through imaging tests. Since the disease is in its earliest phase, this is the best time to take action and slow or even prevent further progression. Patients diagnosed at this stage should have an in-depth discussion with their doctor about lifestyle changes that protect kidney function—including maintaining a healthy weight, managing blood pressure, and keeping blood sugar levels in check (especially for those with diabetes). While no drastic medical interventions are usually required at this point, early consultation with a nephrologist (kidney specialist) can provide valuable guidance on long-term kidney care. With the right approach, many patients can keep their kidneys functioning well for years, if not decades.
Stage Two: The Stealthy Progression
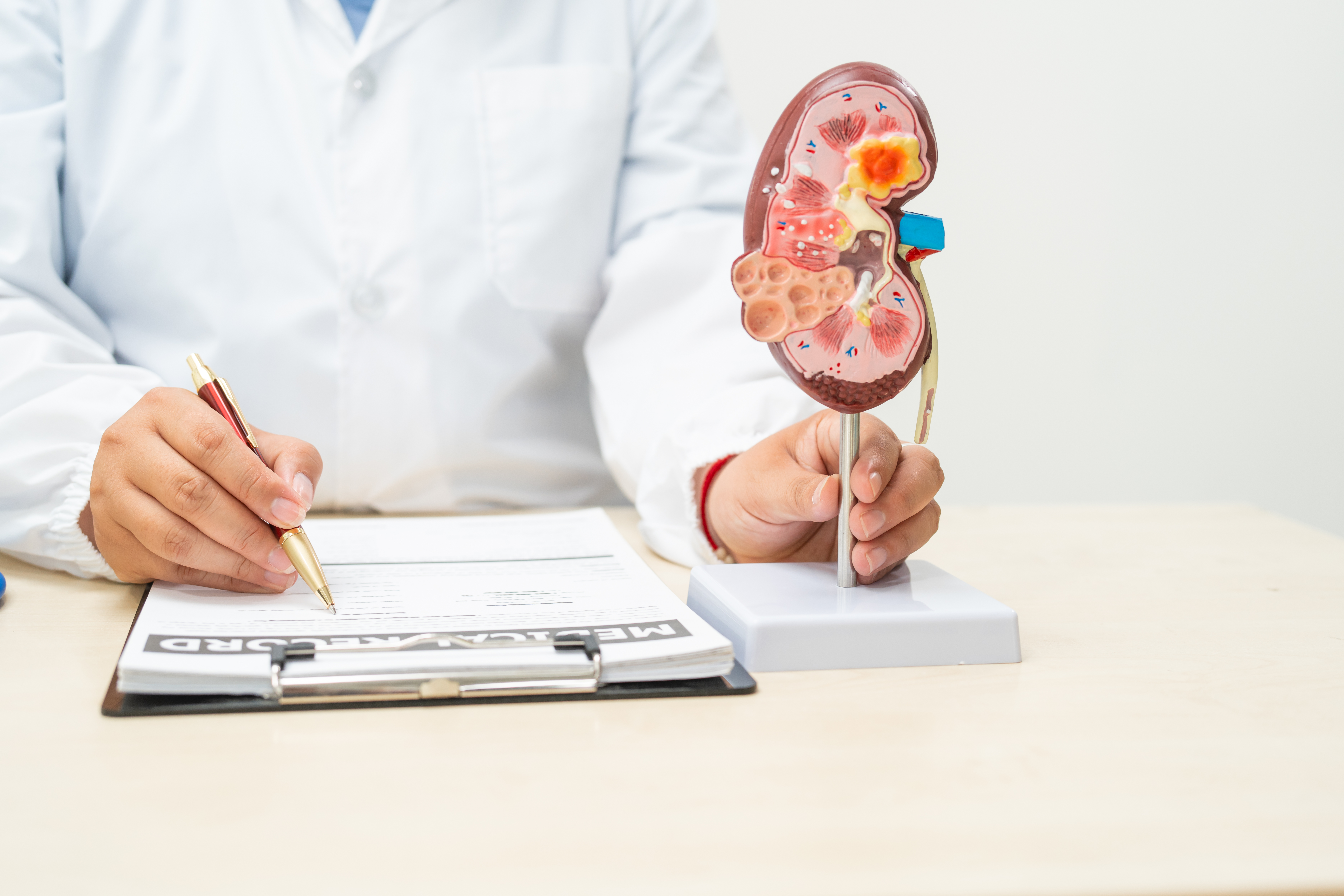
Stage two CKD is still considered mild, and most patients remain asymptomatic, meaning they won’t feel different even though kidney function has begun to decline. A patient is classified as stage two if their eGFR falls between 60 and 89, with lab tests or imaging showing signs of kidney stress. While the kidneys are still filtering waste relatively well, this stage is a crucial window of opportunity to take proactive steps before symptoms develop. Doctors often recommend lifestyle adjustments and medications to slow further damage. Patients at this stage should work with their physician to determine if blood pressure or cholesterol medications (such as ACE inhibitors or ARBs) could help preserve kidney function. Dietary adjustments—such as reducing sodium and protein intake—may also be suggested to ease the burden on the kidneys. Regular blood pressure monitoring at home is highly recommended, as high blood pressure can accelerate kidney decline. Additionally, staying physically active with at least 150 minutes of exercise per week can improve circulation and overall health, benefiting the kidneys. Since CKD at this stage still doesn’t cause symptoms, it’s easy to overlook. However, the choices made at stage two can determine how quickly—or slowly—the disease progresses. Now is the time to take charge of kidney health before the condition becomes harder to manage.
