What Causes A Hemothorax?
When a hemothorax occurs, blood can be found in the pleural space around the lungs. This blood may be coming from the chest wall, lung, heart, or blood vessels. In many cases, a hemothorax remains a result of an injury. A hemothorax must be treated immediately to avoid serious medical consequences. Blood in the thorax region is usually accompanied by excess air around the lungs. So treatment may involve removing both blood and air from the body using a tube inserted into the chest between the ribs. Get to know the various causes of a hemothorax in great detail with this article.
Blunt Force Trauma To The Chest

In many cases, a hemothorax occurs due to an injury or blunt force trauma to the chest. This trauma causes blood to collect in the pleural cavity, which is in between the chest wall and the lungs. Once the blood enters the pleural cavity, it can only be removed by a medical procedure. Even a tiny injury can cause bleeding to happen in the chest wall and lungs and cause a hemothorax. A hemothorax due to trauma may also cause the pleural space to rupture. If an individual has blunt force trauma due to a car accident, altercation, or sports injury, their lungs need to be inspected for possible damage and bleeding.
Improper Blood Clotting
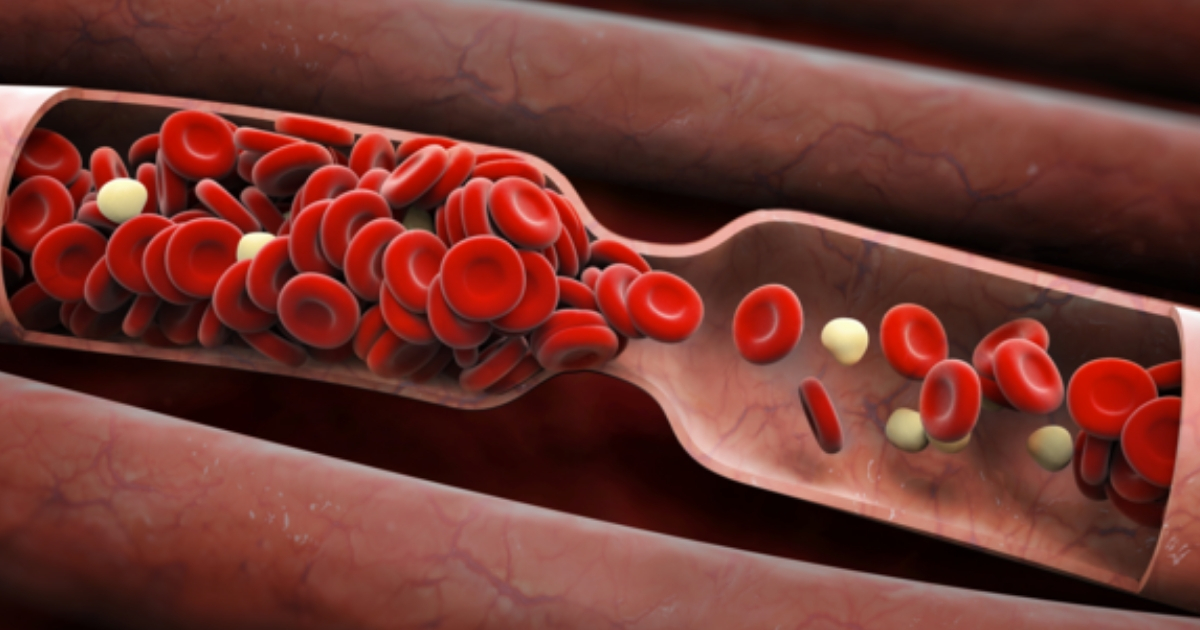
A spontaneous hemothorax can occur in individuals with improper blood clotting issues. Individuals who develop a spontaneous hemothorax may experience symptoms such as chest pain and life-threatening dyspnea. A spontaneous hemothorax may be more likely to happen in patients who take anticoagulant medications or who have hemophilia. A hemothorax may also occur when a plasminogen activator is used for venous thrombosis in pneumonia patients too. Glanzmann thrombasthenia is a genetic disorder that causes clotting abnormalities, which may lead to a hemothorax. Other blood clotting disorders may lead to improper clotting of the blood and hemothorax issues.
