Guide To Treating And Preventing Ventricular Fibrillation
Ventricular fibrillation is an irregular heart rhythm that occurs in the ventricles (lower chambers of the heart). This type of fibrillation is considered a medical emergency and requires immediate treatment. If left untreated, most cases of ventricular fibrillation will lead to cardiac arrest and death. Typically, loss of consciousness is the main symptom of this emergency. Before that, some patients may experience chest pain, rapid heart rate, dizziness, nausea, and shortness of breath. Patients with ventricular fibrillation will not have a pulse, and their electrocardiogram readings will be erratic or completely absent.
Individuals at an increased risk for ventricular fibrillation include those who have previously had a heart attack and individuals with congenital heart defects. Patients who have potassium or other electrolyte imbalances and individuals who have used cocaine or other illegal drugs are also at increased risk. Ventricular fibrillation can be caused by heart failure, cardiomyopathy, shock, long QT syndrome, electrocution, and Brugada syndrome.
Implantable Cardioverter-Defibrillator
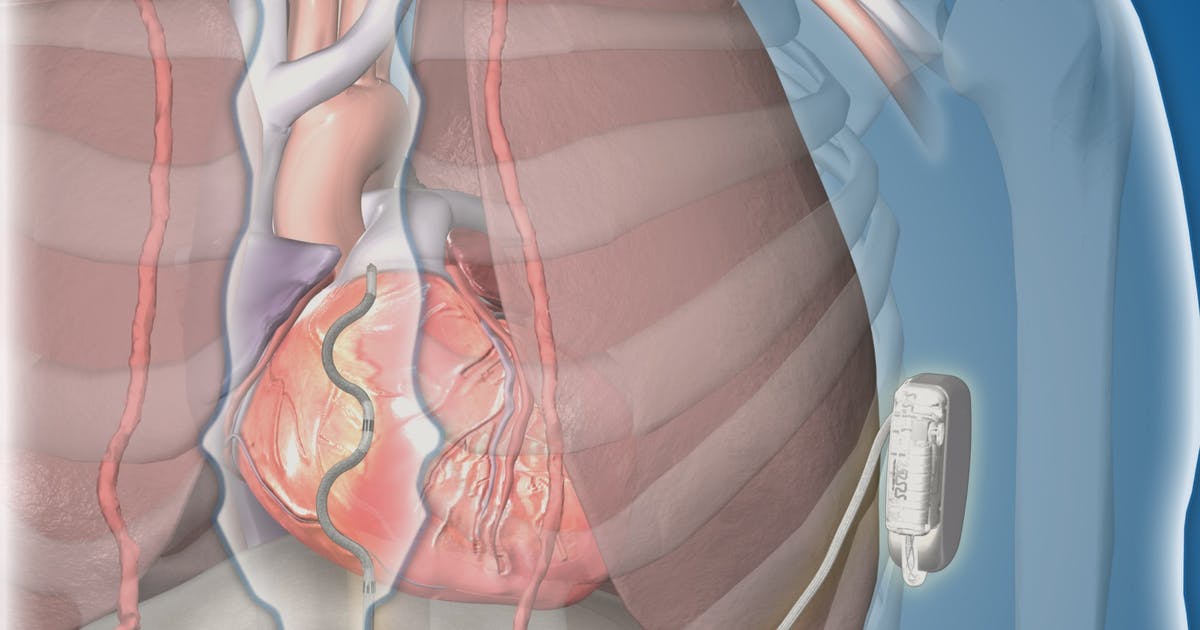
An implantable cardioverter-defibrillator (ICD) is a device that can prevent cardiac arrest and death in patients who have survived previous episodes of ventricular fibrillation. The device is also appropriate for patients who have a high risk of the condition and other types of abnormal heart rhythms. These devices are battery powered, and surgeons place them just underneath the skin, connecting them to the heart muscle through thin wires. They continuously monitor the patient's heart rhythm. If an abnormal rhythm is detected, they will deliver an electric shock to correct this and make the heart beat normally again.
Some implantable cardioverter-defibrillators also serve as pacemakers and can help speed up heart rhythms that are too slow. Patients who have ICDs need to be aware of their surroundings and avoid strong electromagnetic fields; these can prevent the ICD from functioning properly. Patients should also limit or avoid spending time around metal detectors, anti-theft devices, electric fences, and invisible pet fences. When using cell phones and headphones, patients should make sure these are used at least six inches away from their ICD. Cell phone chargers should be used at least twelve inches away from these devices.
Coronary Bypass Surgery

Coronary bypass surgery, which is performed under general anesthesia, can be used to reduce the risk of ventricular fibrillation by increasing blood flow to the heart. Surgeons bypass a damaged blood vessel in the heart, rerouting blood flow with a healthy blood vessel taken from another part of the patient's body. Both open surgery and newer, less invasive methods are available for this operation. Some cases may require open surgery. Following a bypass operation, patients are taken to the intensive care unit, and most stay there for two days. During the first day in intensive care, patients may be on a ventilator that breathes for them, and they may also have a stomach tube, a urinary catheter, an arterial line, chest tubes, and intravenous lines in place.
Most patients can have the majority of these tubes and lines removed on the second day, and they can also begin eating again. On the third day in the hospital, most patients are moved to a regular hospital ward and may stay there for a further two days. After discharge, recovery continues at home, and most patients will be fully recovered in six to eight weeks. Many patients choose to participate in a cardiac rehabilitation program during their recovery. In this program, patients participate in a supervised exercise program and are taught about healthy nutrition.
