How to Treat Catecholaminergic Polymorphic Ventricular Tachycardia
Implantable Cardioverter-Defibrillator
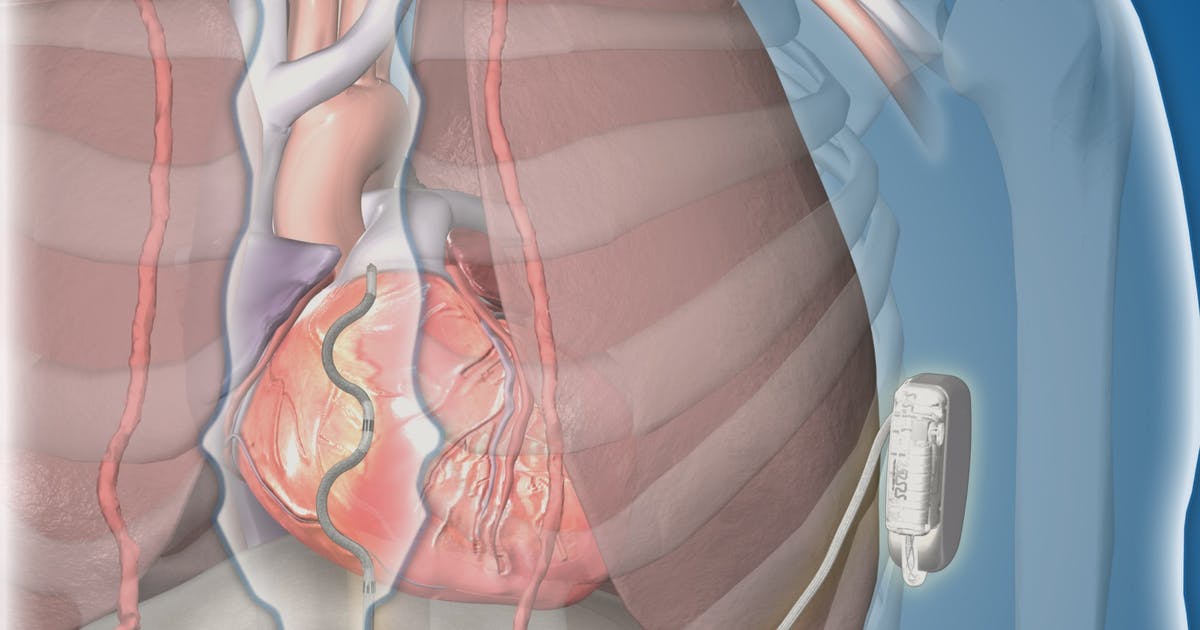
An implantable cardioverter-defibrillator is often advised for patients who have not responded to treatment with medications, and it is typically performed before more invasive treatments. Doctors generally recommend that an implantable cardioverter-defibrillator be considered when patients taking beta blockers continue to have fainting spells or experience an episode of cardiac arrest. Surgeons implant the cardioverter-defibrillator underneath the skin, and thin wires connect the device to the patient's heart. The device continuously monitors the patient's heart rate. If an abnormal rate is detected, the device generates an electric shock that restores the heart to a normal rhythm. Implantable defibrillators are crucial in preventing sudden cardiac death. After having the device placed, patients may need eight weeks to adjust. They may experience jerky arm movements during this time, but these will typically settle after eight weeks. Patients should also watch for any mood changes, depression, or anxiety after surgery and report these to their medical team.
Reveal the next strategy for treating catecholaminergic polymorphic ventricular tachycardia now.
Avoid Strenuous Exercise And Competitive Sports

Patients with catecholaminergic polymorphic ventricular tachycardia often experience fainting, rapid heartbeat, and irregular heart rhythms during and after exercise. Since exercise is such a strong trigger, patients with the disorder are advised to avoid strenuous exercise and competitive sports. Exercise is important for overall cardiac health, but patients with this form of ventricular tachycardia need to involve their doctors in the process of choosing a safe exercise routine. Before starting any exercise regimen, patients should visit their cardiologist for a checkup. The cardiologist can assess the patient's cardiac and overall health. They will listen to the patient's heart and lungs and may perform tests. The patient's cardiologist can recommend types of exercise that are safe and appropriate for each patient. Generally, lighter exercises such as yoga, tai chi, and gentle walking can be safely performed. Doctors will advise patients about safe exercise time limits and how often they should exercise each week. Patients may wish to exercise under the supervision of a personal trainer or join an exercise class for patients with chronic health conditions. Patients may want to monitor their heart rates while exercising.
Discover more ways to effectively treat catecholaminergic polymorphic ventricular tachycardia now.
