Guide To The Causes Of High Liver Enzymes
Statins
Statins are prescription medicines that reduce cholesterol. This type of medication is also routinely prescribed to reduce the risk of heart attacks and strokes in high-risk patients. Research shows that statins can reduce the risk of a second heart attack or stroke by approximately forty percent in patients who have already had one. Atorvastatin, simvastatin, pravastatin, and rosuvastatin are some of the most frequently prescribed statins. During treatment with statins, patients could notice headaches, sleeping difficulties, bloating, abdominal pain, dizziness, and muscle weakness.
Some patients have experienced an increase in liver enzymes while taking statins. This is considered a rare side effect. Taking a low to moderate dose reduces the likelihood of experiencing this effect. Patients will have their liver function carefully monitored during treatment with statins. Individuals with mildly elevated liver enzymes can continue to take the statin they have been prescribed. Patients with moderate to severe elevations may need to change to a different medicine.
Nonalcoholic Fatty Liver Disease
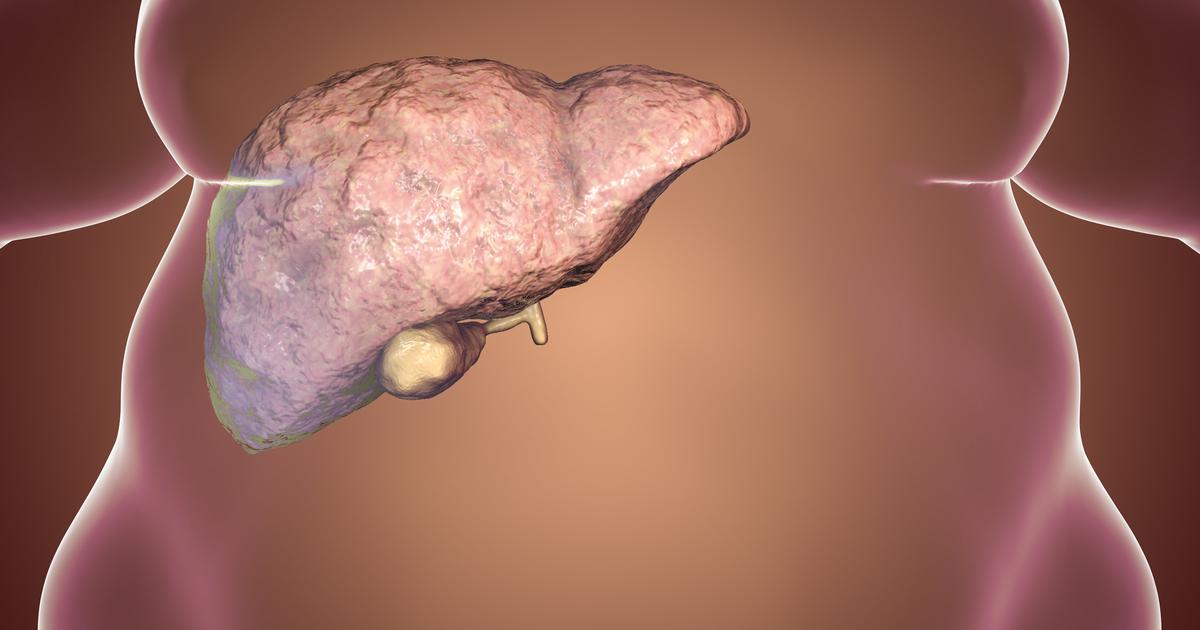
Nonalcoholic fatty liver disease occurs when there is an abnormal accumulation of fat cells in the liver. This condition does not develop due to alcohol consumption. Instead, it is associated with obesity, high blood sugar, high triglycerides, and insulin resistance. Patients with type 2 diabetes, sleep apnea, metabolic syndrome, polycystic ovary syndrome, or high cholesterol have an elevated risk of developing this disease. Usually, this condition does not produce visible symptoms, and most patients are not aware that they have it. The condition may be discovered when routine blood tests are performed for another reason. One of the signs that may be revealed is elevated liver enzymes.
If doctors suspect nonalcoholic fatty liver disease, they may need to do an abdominal ultrasound, CT scans, or a liver biopsy to confirm the diagnosis. Weight loss is the primary treatment for nonalcoholic fatty liver disease. Patients are advised to lose ten percent of their body weight to manage risk factors for the condition. Some individuals notice an improvement in their condition after losing five percent of their body weight. Nonalcoholic fatty liver disease may lead to cirrhosis of the liver. If this occurs, patients might need a liver transplant.
