Guide To The Risk Factors, Causes, And Complications Of Aortic Stenosis
Aortic stenosis refers to a condition in which the aortic valve leaflets do not function properly because they become too stiff to open completely. The aortic valve has to maintain the ability to open fully for blood to exit the heart and flow through the aorta smoothly. When blood does not flow smoothly from the heart into the aorta, the heart muscle must work much harder to pump blood. Symptoms include a heart murmur, dizziness upon exertion, fatigue, appetite loss, chest pain, breathlessness upon exertion, heart palpitations, and poor weight gain. This condition is diagnosed using tests such as a physical exam, echocardiogram, electrocardiogram, stress test, computerized tomography scan, chest x-ray, cardiac MRI, and cardiac catheterization.
Many patients will take medication as part of their aortic stenosis treatment. For instance, high blood pressure medication is quite common. Others will need medication for arrhythmias. Surgery for aortic stenosis is another major treatment option. Most patients need an aortic valve repair or aortic valve replacement. Patients should also practice stress management, get regular exercise, and follow a heart-healthy diet for aortic stenosis. Of course, patients must first understand the various causes and risk factors for this condition, along with complications that appear if it goes untreated.
Calcium Buildup On The Aortic Valve
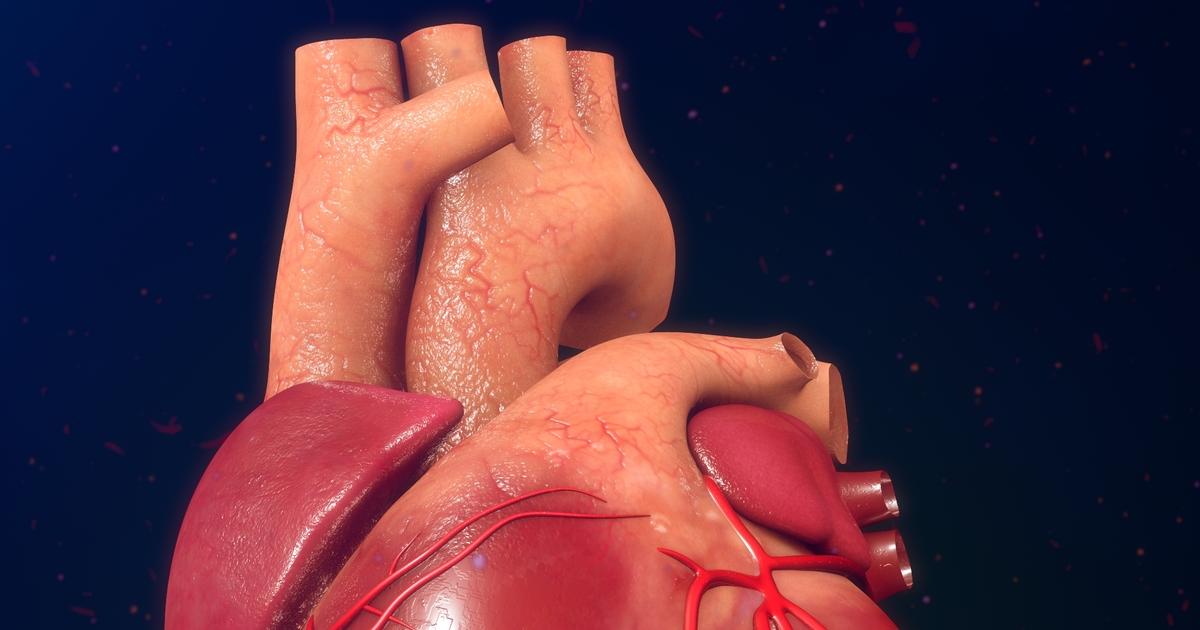
An individual may develop aortic stenosis due to progressive calcium buildup on their aortic valve leaflet tissues. Calcification on the aortic valve occurs when calcium deposits develop in the tissues that make up the valve and its leaflets. An individual in late adulthood or who has coronary artery disease or atherosclerosis is at a higher risk of experiencing the calcium deposits in their aortic valve. The process that causes calcification of the valve tissues is thought to involve a complex interaction between endothelial dysfunction, oxidative stress, and inflammatory responses. These factors cause the remodeling of tissues in the valve and inappropriate disposition of calcium during that process.
As the aortic valve is constantly under significant mechanical stress, it undergoes constant cycles of tissue renewal. Factors like high blood pressure and others that cause mechanical stress on the valve to exceed its ability to remodel and repair itself can cause an impairment of structural integrity. This impairment is further aggravated by the attraction, deposition, and hardening of calcium in the valve that leads to the symptoms of aortic valve stenosis.
Read more about the risk factors and causes of aortic stenosis now.
Rheumatic Fever
An individual may develop aortic valve stenosis from a previous infection referred to as rheumatic fever. This is a disease of inflammation that forms following an untreated or inadequately treated infection of scarlet fever or strep throat. Streptococcus bacteria is what causes scarlet fever and strep throat. Rheumatic fever happens when the bacteria that cause these infections trick a patient's immune system into targeting and attacking its own tissues. The most common tissues in the body that rheumatic fever affects are the central nervous system, heart tissues, and joint tissues.
Aortic valve problems that arise from previous rheumatic fever are known to manifest between ten and twenty years following the initial infection. When the individual's immune system attacks the tissues of the aortic valve because of rheumatic fever, the valve's tissues become inflamed and damaged. The body repairs the damaged and inflamed tissues. However, it does so using scar tissue instead of the same kind of tissue originally in the valve. Scar tissue is more dense and fibrous than normal tissue, which causes the valve to become too stiff, or the condition known as aortic stenosis.
Learn more about the causes and risk factors linked to aortic valve stenosis now.
