Understanding The Causes And Risk Factors For Post-Traumatic Stress Disorder
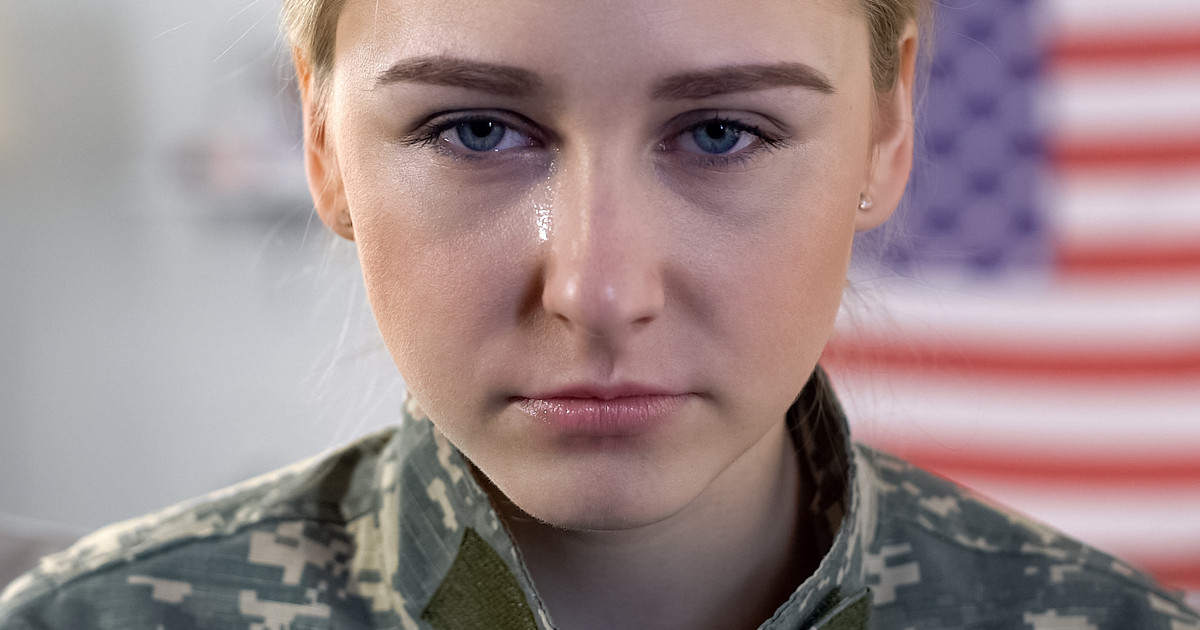
Post-traumatic stress disorder (PTSD) occurs when an individual experiences a traumatic event and following the event, they may experience differences in their emotional responses, heightened anxiety, flashbacks, obsessive thoughts about the event, and other symptoms. The symptoms may start a few days or weeks after the event, but there have been cases where it's years before symptom onset. PTSD is famously seen in war veterans, but nearly a third of the population is estimated to experience at least one traumatic event in their lifetimes.
The actual prevalence of post-traumatic stress disorder is much higher and can occur in anyone. Understanding the causes of PTSD and the risk factors for developing this mental illness will help everyone recognize the symptoms and receive treatment faster.
Stressful Event
The diagnostic criteria for post-traumatic stress disorder specify that an individual can experience symptoms following a single stressful event. However, they might also experience symptoms if they've been exposed to a pattern of stressful or traumatic events. There are several different types of trauma. Sexual and physical assault are two of the most common causes of post-traumatic stress disorder. Emotional abuse and mistreatment can also cause PTSD to develop, particularly in children. Children who experience neglect are more likely to have trauma-induced behaviors later in life, which may include the development of post-traumatic stress disorder.
Illnesses, serious accidents, and frightening medical procedures have also been known to cause PTSD symptoms. Some individuals, particularly children, may develop post-traumatic stress disorder as a result of witnessing domestic violence in their household. It's also possible to develop PTSD after witnessing violence in the community. School violence like fistfights or school shootings can also trigger the development of post-traumatic stress disorder. Some of the other most common reasons include war, political violence, terrorism, natural disasters, forced moving from home, the traumatic loss of a loved one, or trauma caused by the foster care system.
Family History Of Mental Health Issues

Studies have shown a family history of mental health issues will contribute to an individual's likelihood of developing PTSD after a traumatic event. Substance use disorders and mental illnesses both appear to increase the risk. In addition, studies have shown experiencing or witnessing the mental health problems or substance use disorders of family members can in itself lead to post-traumatic stress disorder symptoms. One study showed individuals who had witnessed a physical assault had twice the chances of developing PTSD when someone in the family also had mental health or substance use issues.
For this reason, patients need to talk to their doctor about any family history of mental illness. This includes whether anybody in their family has a substance use problem; experiences depression, anxiety, or other mood disorders; has a personality disorder; or experiences psychotic symptoms. All of these things can increase the risk of post-traumatic stress disorder because of how they affect both an individual's responses growing up and their genetic brain chemistry.
