Guide To Kidney Disease Diagnosis And Treatment
Kidney disease is a condition in which the normal functioning of the kidneys is impaired. As a result, the kidneys are no longer able to filter waste products from the blood as effectively as they should. This condition can be either acute or chronic, and early symptoms may include nausea, vomiting, fatigue, skin itching, swelling of the feet and ankles, and high blood pressure. As the condition progresses, patients may notice shortness of breath or chest pain, and individuals with end-stage symptoms normally require dialysis or a kidney transplant for survival. Patients with diabetes are at an increased risk of developing kidney disease. To diagnose this condition, doctors begin with blood and urine tests, and patients may also need to have an ultrasound exam or a kidney biopsy.
Kidney Biopsy
An individual who has symptoms indicative of kidney disease may need to undergo a kidney biopsy to confirm or rule out a diagnosis. A kidney biopsy is a procedure where a small piece of tissue is removed from a kidney so a pathologist can examine it underneath a microscope. A kidney biopsy is performed by a nephrologist, urologist, transplant surgeon, or interventional radiologist. A kidney biopsy can reveal scarring, immunoglobulin deposits, inflammation, and infection. A kidney biopsy can provide information about how quickly a patient's kidney disease is progressing and how well treatment is working. A kidney biopsy can be performed percutaneously or as an open biopsy. The most common type of kidney biopsy used to diagnose and evaluate kidney disease is a percutaneous biopsy. Open kidney biopsies are performed in special circumstances based on a patient's medical history and physical condition.
Dietary Adjustments

Depending on the stage of a patient's kidney disease, it is often necessary to make a series of dietary adjustments. In general, all patients with kidney disease who are not on dialysis will be asked to reduce their protein intake. Limiting dietary protein reduces the amount of waste products the kidneys must filter. Individuals on dialysis will need to follow a higher protein diet, and they will be guided in this with support from a nutritionist. Patients also need to limit their phosphorus intake. Even for patients in the early stages of kidney disease, phosphorus levels may become elevated, which could result in skin itching and weakening of the bones. To reduce phosphorus levels, patients will be advised to limit dairy products. Individuals in the early stages of kidney disease can generally drink as much fluid as they normally would. However, patients who are in the later stages or those on dialysis will need to carefully monitor their dietary fluids. Excessive amounts of fluid could accumulate in the body in between dialysis sessions, and this may trigger shortness of breath that could become a medical emergency. Patients should ask their dialysis nurse for specific instructions on fluid intake.
Certain Medications
Doctors may prescribe certain medications to help with managing the symptoms of kidney disease. Many patients with this condition have high blood pressure and high cholesterol, and doctors typically prescribe angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers to lower blood pressure. Statins to lower cholesterol may also be necessary, and some patients could be prescribed a diuretic to reduce fluid retention and swelling. Since kidney disease can affect phosphorus levels, patients may be given a phosphate binder to reduce the amount of this mineral in the blood and to protect bone health. Both calcium and vitamin D supplements may be recommended to reduce the risk of bone fractures. Some patients with kidney disease could develop anemia, and this can contribute to the fatigue experienced by individuals with kidney disorders. In these cases, physicians often recommend the use of erythropoietin supplements, possibly with added iron. These supplements help the body produce more red blood cells, which can help patients have more energy.
Dialysis
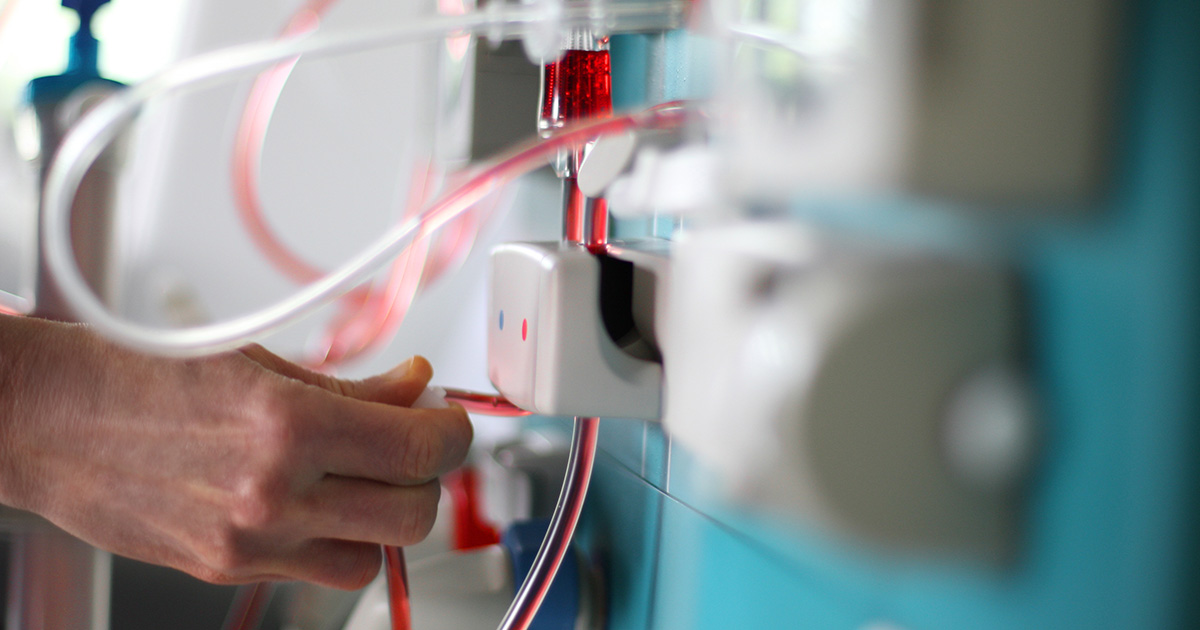
Patients who have progressed to the end stages of kidney disease will require dialysis. In this treatment, waste products and extra fluids are filtered out of the blood through artificial methods. Depending on the patient's health status, they may be offered hemodialysis or peritoneal dialysis. In hemodialysis, the artificial filtration process is completed by a machine. This method is completed at a dialysis center, and each session is about four hours long. Most individuals have sessions at least three times a week. Patients who undergo peritoneal dialysis have a catheter inserted into their abdomen so a specialized dialysis solution can flow into the abdominal cavity. Waste products and excess fluids are absorbed by the solution, and it drains out of the body after four or five hours, taking the absorbed waste and fluids with it. This type of dialysis can sometimes be completed at home. Patients are trained to self-administer the dialysis solution, and the process must be repeated four or five times a day. An automated form of peritoneal dialysis uses a machine, and patients can use this method overnight at home.
Kidney Transplant

A kidney transplant is a surgical procedure that replaces a damaged kidney with a healthy one from a donor. In recommending a kidney transplant, doctors will consider the patient's physical health, mental health, age, and other factors, and patients will need to have medical and psychological assessments. Approved patients will be placed on the transplant list. In many cases, kidney transplants can be completed using live donors. Transplant operations are performed with general anesthesia, and a newly transplanted kidney will usually start producing urine immediately. The hospital recovery period is approximately one week. The incision from the operation heals in roughly six weeks, and patients will need to avoid lifting and exercise other than walking during this period. For the first few weeks or months after a transplant, frequent checkups are necessary, and patients need to remain near the transplant center. Individuals who have had a transplant will also need to take life-long medication to prevent organ rejection.
Exercise Regularly

Patients with kidney disease are often advised to exercise regularly. Frequent physical activity can help in controlling blood pressure, and it also reduces fatigue and stress. Before beginning an exercise program, patients should always ask their physician about which exercises are safe for their health needs. In general, thirty minutes of exercise on five days of the weeks is sufficient. Gentle exercises such as walking, swimming, yoga, tai chi, and dancing can be helpful, and patients may also enjoy doing gardening or household chores for added exercise. Exercising in group classes or with the help of a personal trainer may be beneficial for some patients, too. During exercise, patients should remain vigilant for any chest pain, shortness of breath, or dizziness. If these symptoms occur, patients should stop exercising immediately, and the symptoms should be reported to a doctor.
Quit Smoking And Limit Alcohol

A chronic kidney disease patient will be advised to quit smoking and limit their consumption of alcohol as part of their treatment regimen. Kidney disease develops when the kidney tissues become damaged by some mechanism and can longer meet the demand of the individual's body. Smoking causes harm to the kidneys by increasing their blood pressure, decreasing the flow of blood in the kidneys, increasing angiotensin II production, narrowing blood vessels in the kidneys, causing damage to arterioles, and promoting atherosclerosis in the kidneys. Consumption of alcohol damages the kidneys by altering the way they work to filter toxins and wastes from the blood. An individual who has been diagnosed with kidney disease may be advised to strictly limit their alcohol intake because the impaired kidneys are not able to stop the alcohol from dehydrating the body to harmful levels. Alcohol consumption is also proven to increase blood pressure, which also causes damage to the kidney tissues.
Lose Excess Weight

An overweight or obese individual who has been diagnosed with kidney disease may need to lose excess weight to carry out a successful treatment regimen. Excess weight on the body makes an individual more prone to kidney damage through several known and some unknown mechanisms. Several mechanisms that bridge the association between excess weight on the body and kidney disease are factors in comorbid conditions and diseases that promote kidney disease and are caused by being overweight or obese. These comorbid conditions and diseases include diabetes, atherosclerosis, hypertension, and several others. Excess adiposity in an individual's body increases the production of protein hormones like adiponectin, resistin, and leptin. Excess adipose tissues in the body have direct effects on the functionality of the kidneys through the development of oxidative stress, excessive activation of the renin-angiotensin-aldosterone system, insulin resistance, inflammation, abnormal metabolism of lipids, and increased production of insulin. Losing excess weight in the setting of kidney disease can help slow an affected individual's kidney impairment.
Maintain Healthy Blood Pressure

An individual who is affected by kidney disease may be advised to maintain a healthy blood pressure for their treatment to be effective. Blood pressure is the amount of force of the blood pushing on the walls of blood vessels as it is traveling through them. The blood vessels throughout the body can stretch to accommodate a certain extent of increased blood volume, but they become damaged when the pressure exceeds that threshold. The blood vessel damage induces a repair process by the body to the vessel walls with scar tissue, or tissue that is denser and more fibrous than the original vessel tissues. This scar tissue on blood vessel walls can cause problems with how the blood vessels work around the body and in certain organs like the kidneys. Damaged blood vessels in the kidneys that have accumulated scar tissue are not able to filter extra fluids, toxins, and wastes from the blood like they should be able to. A kidney disease patient must maintain healthy blood pressure to stop their disease from progressing rapidly.
Control Blood Sugar

The most common cause of kidney failure in the United States is diabetes because these patients have uncontrollable high levels of glucose in their blood more frequently than unaffected individuals. High glucose in the blood causes kidneys to be put under twice the workload they would be with healthy blood glucose. In high blood sugar, the kidneys will filter too much blood too quickly, causing the small filters in the kidneys (glomeruli) to become compromised. Proteins in the blood that are important to the body start to leak through the filters and are excreted through the urine inappropriately when the filters in the kidneys are compromised. An individual already affected by kidney disease should carefully manage their blood sugar because even a slight increase in blood sugar and blood pressure can compound the damage to their kidneys.
