Guide To Effective OCD Treatment Options
Obsessive-compulsive disorder (OCD) is a chronic condition characterized by repetitive thoughts and compulsions. It is considered an anxiety disorder, though the symptoms tend to manifest differently than with different identified anxiety disorders. The presentation of symptoms varies widely from person to person. Different individuals will have different obsessions and compulsions, though the two are often linked. For example, if someone is obsessively afraid of being contaminated by germs, they might feel a compulsion to wash their hands repeatedly to lessen their stress. Patients might also have compulsive counting rituals or need to check on things repeatedly to stop obsessing about them. Common examples are needing to check if the door is locked or the stove is off, even if the individual is aware they are.
Uncover common options for OCD now.
Medication

A variety of different medications are used for OCD treatment. If one medication doesn't work, patients might still benefit from one of the others or from switching their dosage. Patients and their doctor need to monitor their thoughts and behaviors to see whether the medication is having a positive effect. Antidepressants tend to be the first OCD medication prescribed. The exact type of antidepressant will vary depending on the patient's symptoms, health, and age. Some of the most common medications to try first are fluvoxamine, fluoxetine, clomipramine, paroxetine, or sertraline. It's important to take the medication on a regular schedule. If the medication is causing side effects the patient doesn't like, they should talk to their doctor about how to safely lower the dose or switch medications. Quitting medication cold turkey might lead patients to have a relapse. If individuals are experiencing suicidal thoughts, they should talk to their doctor, call a helpline, or phone 911, right away.
Keep reading to reveal more options for treating obsessive-compulsive disorder now.
Cognitive Behavioral Therapy

Cognitive behavioral therapy (CBT) is a treatment used for a variety of mental health conditions. In addition to treating OCD, cognitive-behavioral therapy can be used to treat depression, other anxiety disorders, and certain personality disorders. The therapy uses two techniques to help a patient change their thought patterns and behaviors. One is cognitive therapy, and the other is exposure and response prevention. Obsessive-compulsive disorder patients who undergo cognitive behavioral therapy should do so with a therapist who has specific training in OCD. The majority of CBT treatment will be conducted weekly in a therapist's office, though patients will also be given at-home exercises to practice between sessions. Some individuals with severe OCD might need to have more frequent therapy sessions. When undergoing cognitive behavioral therapy, patients learn how to become aware of their thought patterns and combat them. When experiencing the urge to do irrational things, patients are encouraged to lean into the opposite of their desired action. For example, if something makes them feel irrational guilt, they're encouraged to do it again until the guilt response isn't as strong.
Discover additional treatments for OCD now.
Exposure Therapy

Exposure therapy is the main form of psychotherapy used for obsessive-compulsive disorder. Exposure and response prevention (ERP) is a specific subset of cognitive behavioral therapy. Not all CBT therapists are trained in exposure and response prevention, so when individuals seek treatment for OCD, they need to find someone who is. Throughout ERP therapy, patients will slowly be exposed to what triggers their obsessions. They will then be asked to avoid performing the compulsions that typically ease distress and anxiety. A good ERP therapist will move at their patient's pace. They should never be forced or coerced into doing something they don't want to do. To create a treatment plan, patients will need to describe the obsessions and compulsions they face. The patient and their therapist will write them down and arrange them in a list from least to most frightening. As patients start treatment, their therapist will ask them to face one of the fears on their list, starting with the easiest and working their way up.
Read more about how to treat OCD now.
Habit Reversal Training
Habit reversal training is used as a therapeutic technique for a variety of different disorders. On top of OCD, habit reversal training can be used for Tourette's syndrome, pathological skin picking, and compulsive hair-pulling. The first component of this training is awareness training, which is a way of helping the person be more aware of their compulsions, tics, and other behaviors. Awareness training is typically broken down into several steps. After the patient has developed an awareness of when their behavior or tic occurs, their therapist will help them create a competing response, an action that helps replace the impulsive behavior or tic. The competing response tends to oppose the tic, and it can be continued for more than a few minutes. One example would be rather than pulling hair, an individual might curl their hands into fists and hold them firmly at either side of the body. Ideally, the competing action will be one others won't likely notice. To motivate themselves to keep behaviors from recurring, patients are encouraged to list the problems their behavior causes.
Get more details on the best ways to treat obsessive-compulsive disorder now.
Deep Brain Stimulation
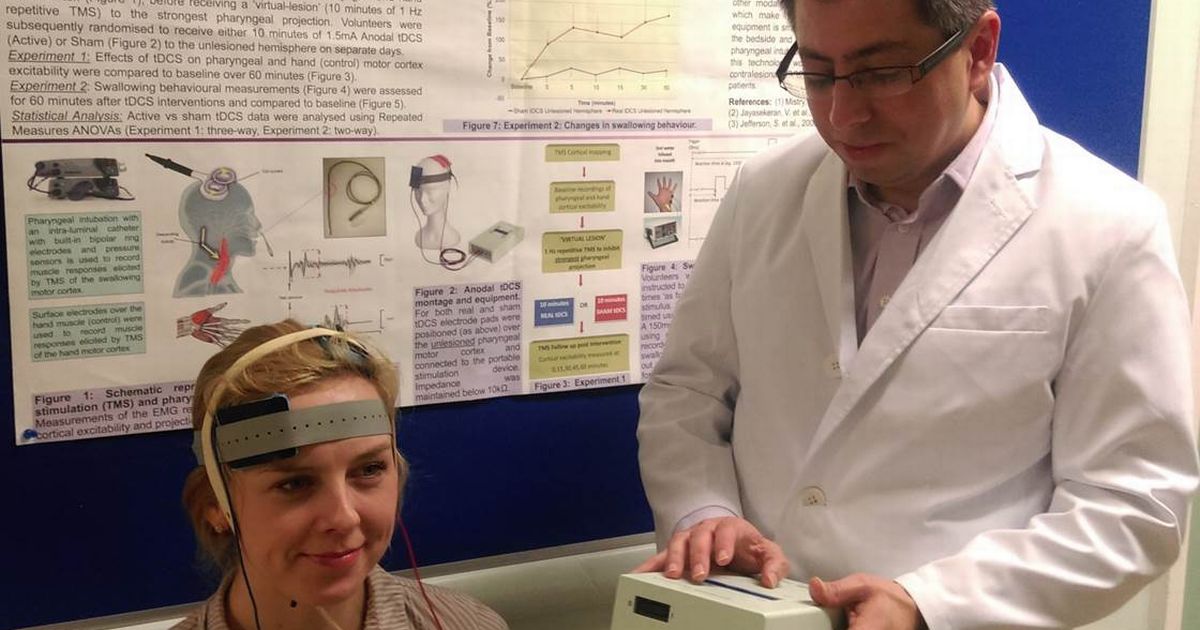
Patients with severe OCD experience all-consuming thoughts and debilitating compulsions that interfere with day-to-day life, and they often experience significant distress. Research indicates deep brain stimulation can be significantly helpful for these symptoms. Deep brain stimulation is recommended for situations where the patient has failed to respond to other treatments. Up to forty percent of obsessive-compulsive disorder patients aren't helped significantly enough by a combination of medication and therapy. Deep brain stimulation has been used to target two parts of the brain involved in OCD: the ventral capsule and the subthalamic nucleus. Before the studies, researchers weren't sure how these parts of the brain influenced obsessive-compulsive disorder or worked together. The study showed VC stimulation helped improve patient mood, while stimulating the STN helped improve the patients' overall cognitive flexibility.
