Guide To Cataract Surgery
Cataracts are a serious eye condition. A cataract occurs when the lens becomes clouded when it should remain clear. This cloudy covering on the lens causes trouble with visual performance, making it difficult to drive a car, see another individual's facial expression, and read. Cataracts develop slowly over several years and usually do not cause any symptoms during the early stages. Common symptoms of cataracts include clouded vision, dim vision, blurred vision, vision problems at night, glare sensitivity, and seeing halos around lights. Others are frequent prescription eyewear alterations, yellowing of colors, and double vision in one eye.
Many patients will wear prescription glasses for cataracts. They are the best non-surgical treatment for cataracts. Although many individuals may want a natural cataract treatment, the best option is surgery. Surgery is quite effective, and doctors may even use laser eye treatment for cataracts as part of the procedure. Of course, patients must understand cataract surgery before they undergo it.
When It Is Performed
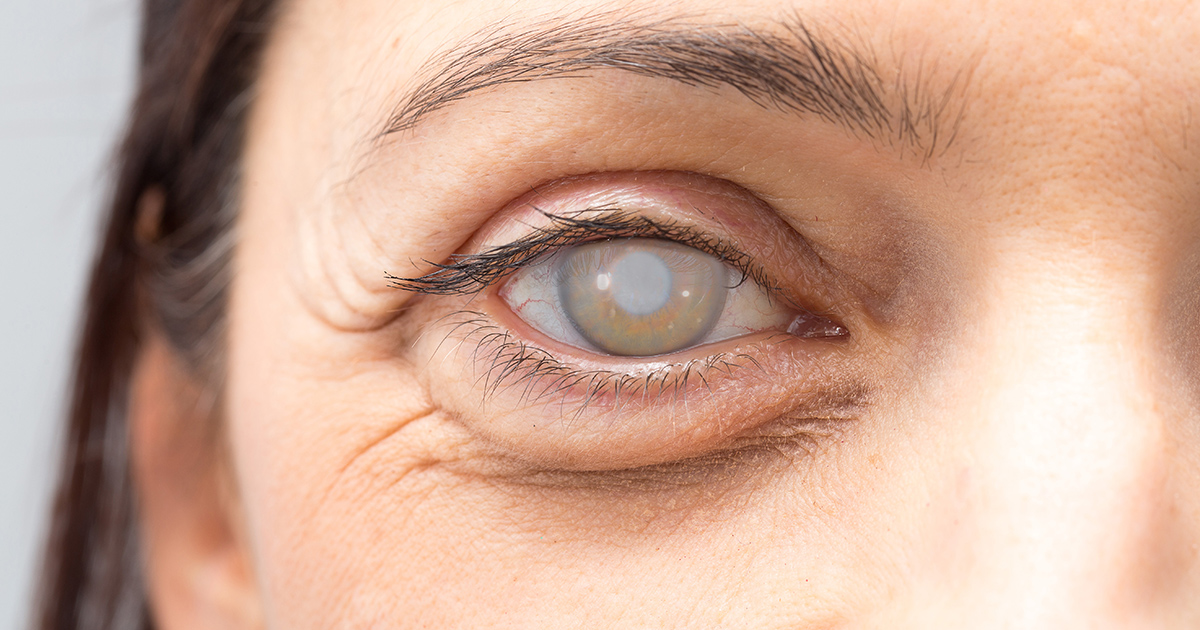
Cataract surgery is a common medical procedure because cataracts are one of the most prevalent causes of visual impairment in individuals over sixty years old. This type of surgery is performed on a patient who has cataracts that have progressed so much that other treatments are no longer effective. The surgery is needed when vision problems disrupt an individual's everyday life and activities. In some cases, the presence of cataracts can cause problems with the treatment of another eye problem. Examples of these eye problems are diabetic retinopathy and age-related macular degeneration.
Surgery becomes necessary when other eye conditions cannot be treated due to cataracts. Cataract surgery is often performed at the same time as another eye surgery because it is more convenient. Another reason is that cataracts have to be removed to complete the other eye procedure.
Preparing For Surgery

Patients can prepare for cataract surgery in several ways to ensure their procedure and recovery go smoothly. The doctor will often perform an ultrasound to evaluate the shape and size of the patient's eye a week before the surgery. The patient will need to arrange transportation to and from the facility where the procedure will take place. Patients taking certain medications may be advised to stop taking them several days before their surgery. These medications include anticoagulants, antiplatelets, acetylsalicylic acid, and some stimulants.
Most patients must refrain from eating or drinking anything during the twelve hours before their surgery. The night before the surgery, patients may be given eye drops or other medications. They must follow specific instructions for these drops. An individual will be advised not to consume any alcoholic beverages the night before they have cataract surgery. Some patients may be prescribed a medication to take the night before the procedure if they are too anxious to get the proper amount of sleep.
How The Procedure Works

The surgery used to remove cataracts typically takes around an hour to complete. The surgeon will first give the patient drops in their eye to help dilate or enlarge their pupils. A patient may receive sedatives to help relax them before the local anesthetic is administered. There are two different methods a surgeon can use to remove the clouded lens. Phacoemulsification is a method where the surgeon makes a corneal incision and inserts a specialized and thin probe into the part of the lens where the cataract is located. The probe is then used to emulsify or break up the cataract with ultrasound waves before the leftover fragments are suctioned out of the eye.
Extracapsular cataract extraction is where the surgeon makes a larger incision and removes the front capsule of the lens that contains the cataract. The back of the lens capsule is left undisturbed so it can function as a resting surface for the artificial lens. Once the lens is placed, the surgeon stitches the incision. Extracapsular cataract extraction is reserved for patients who are not suitable candidates for phacoemulsification.
Choosing An Intraocular Lens

During cataract surgery, the doctor will insert an intraocular lens to replace the clouded part that they remove. This artificial lens is permanent, which makes it quite different from contact lenses. There are a variety of different intraocular lenses available for patients. The most common is the monofocal intraocular lens. This lens is fixed and stays at one distance. This means that if a patient's monofocal lens is for distance vision, they will often need to wear reading glasses or similar glasses to see close items. A multifocal lens, however, acts quite similar to progressive or bifocal glasses. This means that this intraocular lens helps individuals see at several distances. However, it takes patients longer to adjust to this type of intraocular lens. In addition, patients are more likely to see glare or halos around lights with a multifocal lens.
Patients will often receive a toric intraocular lens during cataract surgery if they also have astigmatism. This is to lessen astigmatism to avoid the need for glasses after surgery. Another type of intraocular lens offered during cataract surgery is an accomodating intraocular lens. This type acts more like an individual's natural lens. It will focus at multiple distances and makes the need for reading glasses less likely. Ultimately, it is vital for patients to discuss their options in detail with their doctor.
Anesthesia During Surgery

In most cases, individuals will receive local anesthesia during surgery for cataracts. This is done for several reasons. One of these reasons is that the surgery itself tends to take less than an hour, which lowers the need for general anesthesia. In addition, using local anesthesia lowers the risks associated with anesthesia. Patients may have choices in their local anesthesia. Some of them will be able to have topical eye drops to numb their eye for the procedure. Others may wish to have an injection to block their nerves around the area. Patients may also receive intravenous medication before the cataract surgery to keep them calm.
Overall, local anesthesia will keep patients comfortable and often leaves them with little memory of the surgery. Of course, some patients may require general anesthesia during their cataract surgery. This form of anesthesia is often reserved for extremely anxious patients and those who will have trouble remaining still during the procedure, such as individuals with Parkinson's disease.
Risks Of The Procedure
Just like any other medical procedure, surgery to remove cataracts carries some risk of certain complications. Patients are at a higher risk of complications if they have a preexisting eye condition or disease unrelated to their cataracts. Another underlying condition, like macular degeneration, can cause a patient's cataract surgery to be unsuccessful at improving visual performance. A patient may experience the common side effects of inflammation, swelling, and infection in their eyes after they have the procedure.
Uncommon complications include bleeding, drooping eyelid, retinal detachment, development of a secondary cataract, dislocation of an artificial lens, glaucoma, and vision loss. Taking all of the recommended precautions and making all of the necessary pre-procedural preparations can help patients avoid increasing their risk of complications.
Posterior Capsule Opacification

The most common complication that follows cataract surgery is posterior capsule opacification. This complication may be referred to as a secondary cataract. However, this is not the case. After surgery, the patient's vision should be clear. Unfortunately, this complication changes that. It causes the posterior part of the lens capsule to become hazy. The reason that this happens is that leftover cells grow over the back of the capsule. This growth thickens the capsule and makes it become cloudy. This will happen over time and results in blurry vision. Some patients may have issues with glare and bright lights.
In most cases, posterior capsule opacification occurs in a few months or years after patients receive cataract surgery. Certain patients are more likely to experience this complication. Younger patients are more likely to develop it. In addition, eye inflammation and conditions such as retinitis pigmentosa also increase an individual's risk. However, even without risk factors, posterior capsule opacification is common. It occurs in approximately twenty percent of all patients who receive cataract surgery. Thankfully, laser treatment can cure this complication.
Recovery Process
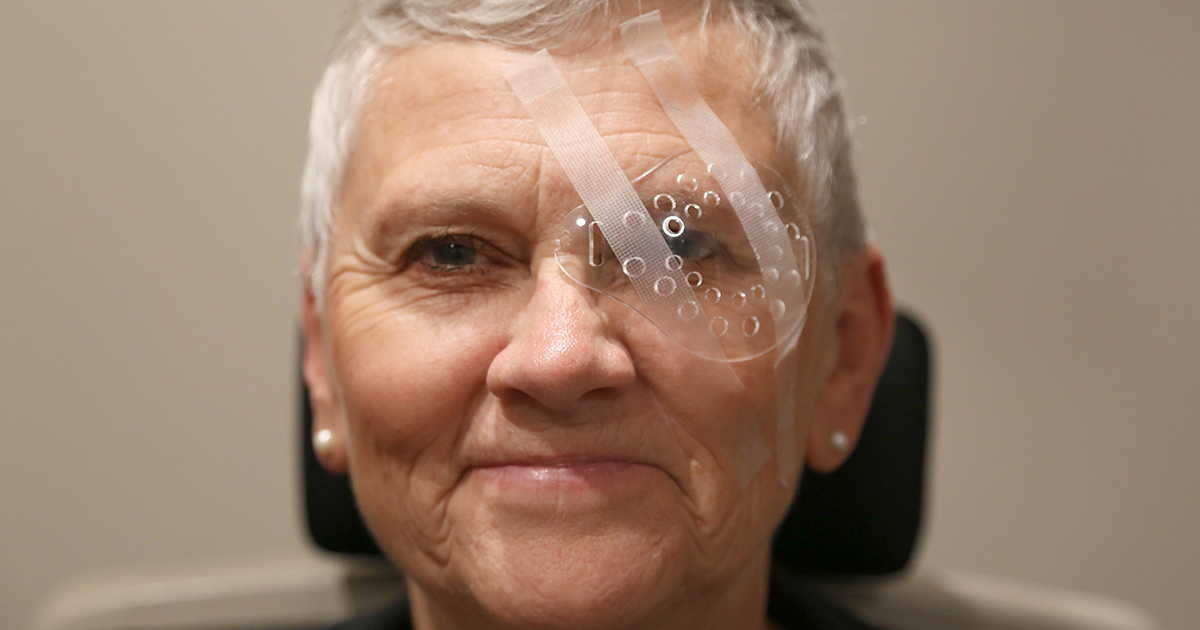
Patients may experience blurry vision in the first few days after their cataract surgery. Visual performance in a patient who has just had cataract surgery should improve within five days. Most patients report colors are brighter and more defined after they have had their cataracts removed. Patients should expect Itchiness and mild discomfort during the first few days after cataract surgery. They should avoid touching, rubbing, or pushing on their eye for five days following their procedure. Most individuals must wear a patch over their eye for the rest of the day and when sleeping for a week.
Prescription eye drops may be given to a patient who has had cataract surgery to help prevent the development of a post-procedural infection in the eye. Eye drops may also be prescribed to keep the pressure inside of the eye at an acceptable level and reduce inflammation in the eye. It takes around eight weeks for a patient to recover fully from their cataract surgery. Patients may need to get prescription glasses between one and three months following their cataract surgery.
Glasses And Cataract Surgery

As mentioned, many patients with cataracts wear prescription glasses before their surgery. This is to correct their vision. However, prescription glasses do not effectively treat severe cataracts. This is why patients need surgery. It is also worth noting that some patients will still need to wear glasses after their surgery. For instance, patients who choose intraocular lens implantation with their standard surgery will often need to wear reading glasses. They may also need computer glasses or other types for specific uses. It varies depending on the patient's specific needs.
Patients may also want to have a pair of progressive lenses to cover a variety of situations. These lenses allow them to see at all distances. Of course, most patients need to wear special glasses during their recovery. Ultimately, patients will need to review their need for glasses with a doctor or optometrist after their surgery.
Follow-Up Appointments After Surgery

Cataract surgery is an outpatient procedure, which means that patients will be able to go home the same day. However, patients will need to have follow-up appointments with their eye doctor. The exact schedule can vary based on the patient and their needs. Of course, there is a standard schedule that most doctors will recommend. This includes a follow-up appointment one or two days after the surgery, one a week later, and then one a month after that.
These appointments will help patients through the recovery process and check on how their vision is improving. These appointments also help doctors address any issues during the patient's recovery, including prescribing additional medications for pain, dealing with complications, and assessing the need for glasses.